Foot Pathology: Infection
Infection in the foot can result from various sources, including direct implantation, hematogenous spread and contiguous extension, as occurs with diabetic foot ulcers. Surgery and trauma may cause direct implantation. Puncture wounds occur commonly in children who walk barefoot, and “osteomyelitis of the os calcus” has been described as a complication of repeated heel puncture for blood samples in infants. Although the plantar surface of the foot is often the portal of entry for directly implanted infection, the infection can spread across fascial planes into other foot compartments. Ledermann et al. evaluated MR studies of the foot to determine if the spread of infection in the foot was limited by fascial planes. Their results show that there were specific propensities for the spread of infection across fascial planes, depending on the origin of the infection. Infection beginning in the toes spread proximally to the forefoot in 34%, and in 18% more than 1 forefoot compartment was involved. Infection originating in the forefoot and midfoot spread to the toes in 68% of cases, with proximal spread of infection from these sources much less common. Pedal infection spread across fascial planes in 30% of infections originating in the medial compartment, in 44% of those that originated in the central compartment, and 80% of those arising in the lateral compartment. Hindfoot infection, which most commonly occurred in the setting of a heel ulcer, did not generally spread across fascial planes.
Foot infection is classified by the anatomic region involved. Imaging is integral to delineate the anatomy affected : subcutaneous tissue (cellulitis), tendons and/or tendon sheath (tendonitis), bursa (septic bursitis), deep soft tissues (fasciitis), bone (osteomyelitis) or joint (septic arthritis)(5). It has been shown in diabetics with foot ulcers that the presence of abscess, gangrene and/or osteomyelitis correlates with a worse outcome and substantially higher likelihood of the need for amputation (14), underscoring the properly characterizing the specific anatomic regions involved by infection.
In diabetics, foot ulcers are usually to source of an infection. An MR study of diabetic feet described the distribution of foot ulcers in 120 sites of skin breakdown. The most common were the skin adjacent to the 5th metatarsal, the skin adjacent to the 1st metatarsal, the skin overlying the distal phalanx of the 1st toe . The ulcers are common below the metatarsal heads and in the distal toes, but may also be identified under the calcaneus and over malleoli. Although pedal infection typically arises from the region of an ulcer in diabetics. ischemic ulcers do not always develop infection.
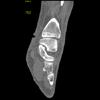
Cellulitis is defined as superficial soft tissue infection (Figure: CT of cellulitis). CT may be required to exclude the presence residual foreign body. The distinction from fasciitis must be made by imaging in some cases. The latter requires surgery, and is seen in older patients with underlying diseases such as diabetes, cancer, drug or alcohol abuse, chronic renal failure and malnutrition. On MR, cellulitis is seen as subcutaneous thickening and fluid, with superficial enhancement. Necrotizing fasciitis manifests as deep fascial fluid and thickening, with deep fascial enhancement. MR has been shown to be accurate for identifying fasciitis, and the criteria described are similar to those used for CT distinction. In one CT series of necrotizing fasciitis in various locations, asymmetric fascial thickening (seen in 80%) and soft tissue gas (seen in 55%) were two important indications of the presence of necrotizing fasciitis. CT is particularly helpful in its ability to unequivocally demonstrate deep soft tissue gas (Figure: CT of necrotizing fasciitis (gangrene)). Focal fluid collections or abscesses can be seen, and fat infiltration is common.
MR has also been helpful in describing the appearance and location of pedal abscesses. The data from one study is very helpful regardless of the imaging modality used to evaluate the foot in diabetics. Abscesses were present in 18% of cases of advanced infection in this series, 90% of whom were diabetic patients. The abscesses occurred most commonly in the forefoot (47%), but were also seen in the hindfoot (22%) , toes (9%), midfoot (13%) and multiple locations in (9%). Nearly all of them (97%) arose near a skin ulcer. Pedal abscesses were significantly more common in the presence of osteomyelitis (97%) and post operatively (33%).
Soft tissue infection in the foot can spread to tendons, as described in another MR study of the infected foot. This may occur in forefoot infection (43%, flexors more common than extensors) and in hindfoot infection (44%, Achilles tendon most common). This study showed that approximately 50% of those undergoing surgery for pedal infection had tendon involvement, and preoperative detection can alter the surgical management. On MR, the criteria used to detect tendonitis were peritendinous contrast enhancement of a tendon directly contiguous to a skin ulcer or cellulitis. If a MDCT study is performed with IV contrast, careful evaluation of the tendons should be performed.
If contrast is administered, it is also important to search for regions of nonenhancing tissue. MR has shown that in the setting of pedal infections in diabetics, regions of nonenhancing tissue were proven to be necrotic tissue at surgery. Septic arthritis has been reported to occur in 33% of cases pedal infection where osteomyelitis was suspected. The most common joints involved in one series were the 1st and 5th metatarsal phalangeal joints in the forefoot. Joint infection was usually located near skin ulcers and osteomyelitis. The 2nd ray was most commonly affected, followed by the 1st and 5th. Findings of septic arthritis include narrowing of the joint space, lytic lesions both centrally and marginally located, bone destruction and periosteal reaction.
One of the primary indications for CT of the infected foot is the detection or exclusion of osteomyelitis. In one study comparing CT to MR, MR was determined to have a higher sensitivity and accuracy for osteomyelitis (sensitivity: 94% vs. 66%; accuracy 93% vs. 80%), although CT was slightly more specificity (MR: 93%; CT: 97%, not significant). Nonetheless, CT is excellent for depicting cortical bone and detecting the findings of erosions, lysis and periostitis (Figure: CT of osteomyelitis). CT can delineate the extent of bony infection and evaluate for medullary involvement. In chronic osteomyelitis, CT is very helpful for detecting sequestra, abscesses and foreign bodies, and is useful to guide the operative approach in the cases which require surgery.
In the foot, the distribution of bones typically involved by osteomyelitis has been described. Nearly 90% of bone infection arises adjacent to infected foot ulcers. Of the toes, the 1st and 2nd are most commonly involved, and of the rays the 1st and 5th are most commonly affected. In the hindfoot, the calcaneus was the bone most commonly infected, due to the anatomic proximity to the most common site of hindfoot ulceration, the heel.
 | 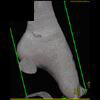 |  | 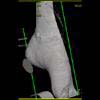 |
Diagnosis: Ankle ulcer. | |||
