Imaging Pearls ❯ Syndromes in CT ❯ Tuberous Sclerosis
|
-- OR -- |
|
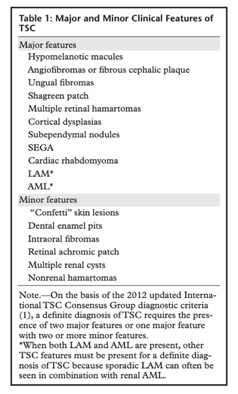
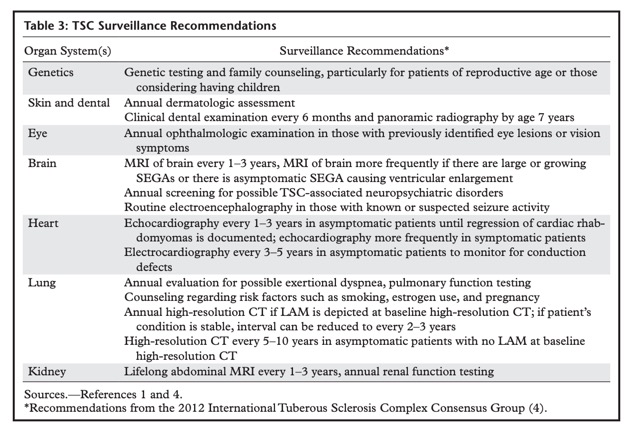
- “Tuberous sclerosis complex (TSC) is a relatively rare autosomal dominant neurocutaneous disorder secondary to mutations in the TSC1 or TSC2 tumor suppressor genes. Although manifestation of the classic triad of seizures, intellectual disability, and facial angiofibromas may facilitate timely diagnosis of TSC, the multisystem features that may indicate TSC in the absence of these manifestations remain highly variable. In addition, patients with TSC are at risk of developing multiple benign and malignant tumors in various organ systems, resulting in increased morbidity and mortality.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “Key manifestations include cortical dysplasias, subependymal nodules, subependymal giant cell astrocytomas, cardiac rhabdomyomas, lymphangioleiomyomatosis, and angiomyolipomas. Renal angiomyolipomas in particular can manifest with imaging features that mimic renal malignancy and pose a diagnostic dilemma. Other manifestations include dermatologic and ophthalmic manifestations, renal cysts, renal cell carcinomas, multifocal micronodular pneumocyte hyperplasia, splenic hamartomas, and other rare tumors such as perivascular epithelioid tumors.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “Renal AMLs represent the second most frequent cause of morbidity among patients with TSC owing to the risk of spontaneous hemorrhage and rupture. Such complications occur increasingly with AMLs that are larger than 4 cm or with those that are associated with aneurysms larger than 5 mm. If either of these criteria is met, embolization or nephron-sparing surgery is highly recommended.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “TSC is an autosomal dominant disorder with a highly variable phenotype and a relatively rare estimated prevalence: one in 10 000 persons . Two-thirds of cases are sporadic and secondary to de novo mutations. Genetic linkage is related to loss-of-function germline mutations in the tumor-suppressor gene TSC1 or TSC2. The TSC protein complex TSC1 at the 9q32 locus encodes hamartin, while TSC protein complex TSC2 at the 16p13.3 locus encodes tuberin.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 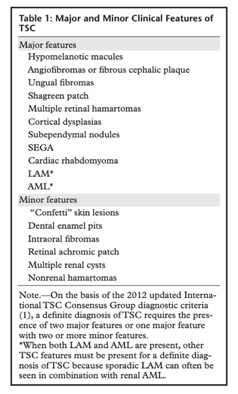
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010- “Cardiac rhabdomyomas are considered a major feature of TSC. They manifest in up to 80% of TSC cases and are rarely seen in persons who do not have this disease. Therefore, TSC should be suspected if cardiac rhabdomyomas are identified. The majority (90%) of persons with TSC are found to have multiple rhabdomyomas after they present. At gross pathologic examination, cardiac rhabdomyomas are well-circumscribed nonencapsulated masses with diameters ranging from 2 to 20 mm. These benign tumors are characterized by irregular myocyte architecture, including “spider”cells, which are so named because of their unique cytoplasmic extensions.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “LAM is the most common pulmonary manifestation of TSC, occurring in 26%–57% of affected patients. LAM occurs as a result of proliferation of smooth muscle cells throughout the peribronchial, perivascular, and perilymphatic regions of the lung. This entity belongs to the PEComa family, which also includes AML. It should be noted that LAM may also occur sporadically and needs to be distinguished from TSCassociated LAM. Sporadic LAM occurs almost exclusively in women; in contrast, TSC-associated LAM may occur in men in 10%–38% of cases.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “Similar to LAM, AMLs are mesenchymal tumors categorized under the PEComa family of neoplasms. These tumors originate from clonal proliferation of epithelioid cells located around blood vessels. AMLs may be found in multiple organs, most notably the kidneys, and the presence of two or more of these tumors is considered a major feature of TSC. Renal AMLs can be identified in 55%–75% of patients with TSC. They are often discovered incidentally owing to their asymptomatic nature; however, they can manifest with abdominal pain, hematuria, anemia, hypertension, and/or retroperitoneal hemorrhage. Renal AMLs can multiply and grow during puberty, suggesting an estrogenic influence.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “There are two histologic subtypes of AML: classic and epithelioid. At gross pathologic examination, classic AML appears as a well-defined expansile mass in the renal cortex or medulla. Tortuous vasculature, clear to eosinophilic cells, and spindle cells are visible at microscopy. Epithelioid AMLs occur more frequently in patients with TSC (27%) than in the general population (7%). Malignant transformation of epithelioid AMLs can occur and may be suspected in the presence of rapid growth or necrosis. In contrast, classic AMLs tend to remain benign.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “The hallmark finding of lipid-rich AML is the presence of intratumoral fat with an attenuation of −10 HU or lower on noncontrast CT images. These tumors demonstrate variable enhancement. It should be noted that RCC may rarely demonstrate a small amount of intratumoral fat, and this is a potential cause of diagnostic dilemmas. The presence of calcification within a fat-containing renal mass should alert the clinician to the diagnosis of RCC. In contrast, calcification is extremely rare in AML.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “Renal AMLs represent the second most frequent cause of morbidity among patients with TSC owing to the risk of spontaneous hemorrhage and rupture. Such complications occur increasingly with AMLs that are larger than 4 cm or those that are associated with aneurysms larger than 5 mm. If either of these criteria is met, embolization or nephron sparing surgery is highly recommended. Tumors that do not fulfill this criterion are followed up conservatively or treated with mTOR inhibitors, elective embolization, ablative therapies, or nephron-sparing surgery.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “Renal cysts are the second most prevalent renal feature of TSC, occurring in 17%–47% of pediatric patients with TSC. Because of their low specificity, multiple renal cysts are considered a minor feature of TSC. TSC-related renal cysts can appear with varying severity, from microscopic disease to a serious polycystic variation. The polycystic variation occurs in about 2%–3% of patients with TSC and results from contiguous mutations of TSC2 and polycystic kidney disease type 1 (PKD1) genes, which are located close to each other on chromosome 16p13.3.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “RCC occurs in only 2%–3% of persons with TSC, similar to its prevalence in the general population. However, unlike sporadic RCC, TSC-related RCC occurs in comparatively young individuals—in whom the median age at diagnosis is 28 years—and tends to be less aggressive . TSC-related RCC can be categorized into three major histologic subtypes: papillary, chromophobe, and clear cell. These subtypes tend to exhibit different imaging patterns owing to their varying histologic components..”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 - “Hepatic AML is a relatively common benign feature of TSC, occurring in 16%–24% of TSC cases. These neoplasms are frequently multiple and may be seen in patients with coexisting renal AMLs. Hepatic AMLs are generally asymptomatic, but they may manifest with abdominal pain or an abdominal mass. At gross pathologic examination, they are characterized by a heterogeneous mixture of smooth muscle, adipose tissue, and vascular tissue. Because of their varying compositions, hepatic AMLs have heterogeneous imaging appearances On contrast-enhanced US, CT, and MR images, the majority of these neoplasms demonstrate hypervascularity during the arterial phase and sustained enhancement during subsequent phases.”
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010 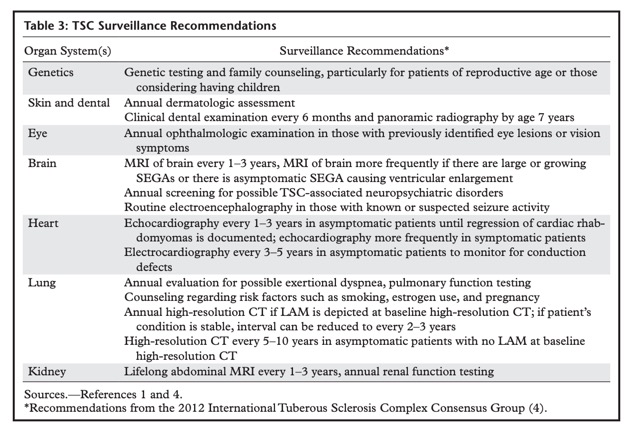
Tuberous Sclerosis: Current Update
Wang MX et al.
RadioGraphics 2021; 41:1992–2010