Imaging Pearls ❯ Spleen ❯ Infection and Infarction
|
-- OR -- |
|
- “Sarcoidosis is a systemic inflammatory condition characterized by noncaseating granulomas. Its annual incidence ranges from 1 to 15 per 100,000 individuals and is more common in women. While pulmonary and mediastinal lymph node involvement is common, affecting 90% of patients, splenic involvement is reported in close to 24% of cases. Splenic sarcoidosis at CT scans reveals multiple solid hypodense nodules of varying sizes, typically hypoenhancing after contrast administration, often coexisting with hepatic nodules and abdominal lymphadenopathies . Traditionally, these splenic lesions exhibit characteristic MRI features based on disease activity. Inflammatory lesions show high signals on T2 and DWI sequences, whereas fibrous lesions present with low signals on both T1 and T2 sequences.”
Spleen anomalies and lesions in CT and MRI: essentials for radiologists and clinicians—a pictorial review
Andres Felipe Herrera‑Ortiz et al.
Abdominal Radiology 2024 (in press) https://doi.org/10.1007/s00261-024-04405-6 - Splenic metastases are rare and often associated with advanced stages of widespread metastatic disease in melanoma,breast, ovarian, lung, and colon cancers . Splenic metastases are generally multiple, although isolated metastasis has also been reported as an even rarer occurrence. At CT, splenic metastases commonly present as hypodense lesions; nevertheless, their appearance can vary based on the primary tumor, occasionally manifesting as cystic lesions with diverse enhancement patterns. At MRI, splenic metastases present low signal intensity on T1 and high signal intensity on T2 sequences, with a variable degree of contrast enhancement, making their diagnosis challenging.
Spleen anomalies and lesions in CT and MRI: essentials for radiologists and clinicians—a pictorial review
Andres Felipe Herrera‑Ortiz et al.
Abdominal Radiology 2024 (in press) https://doi.org/10.1007/s00261-024-04405-6 - Primary splenic angiosarcoma predominantly affects patients in the 6th–7th decade of life, with an annual incidence of one case per 4 million individuals. This aggressive neoplasm displays a predilection for males and has a poor prognosis, marked by a high mortality rate and significant risk of rupture in up to 30% of cases. At CT imaging, splenic angiosarcoma often presents as solitary or multiple poorly defined nodular masses distorting the normal anatomy of the spleen and producing enlargement. The contrast enhancement pattern on CT varies depending on the extent of necrosis within the lesion. Its enhancement is usually centripetal and heterogeneous, and 69–100% of the cases tend to present with metastases, most commonly disseminating to the liver, lungs, adrenals, bones, and lymphatics .
Spleen anomalies and lesions in CT and MRI: essentials for radiologists and clinicians—a pictorial review
Andres Felipe Herrera‑Ortiz et al.
Abdominal Radiology 2024 (in press) https://doi.org/10.1007/s00261-024-04405-6
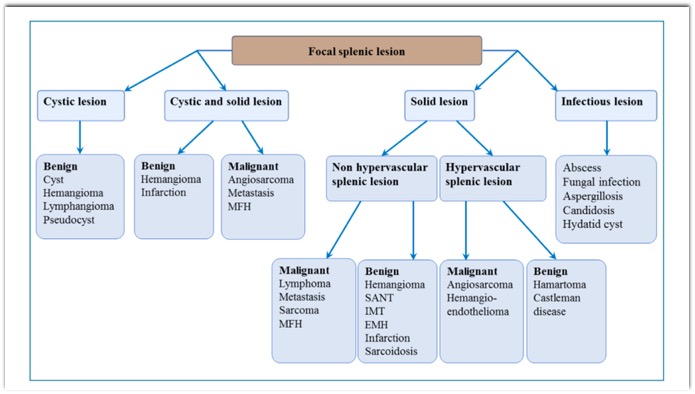
Diagnosis and treatment of focal splenic lesions
B. Malgras, H. Najah, A. Dohan et al.,
Journal of Visceral Surgery, https://doi.org/10.1016/j.jviscsurg.2021.11.010- “ Pyogenic Splenic abscess is most often due to hematogenous spread of infection with risk factors of diabetes, immunosuppression, corticosteroid therapy and sickle cell disease. It usually manifests as a high fever with chills and pain in the left hypochondrium. Splenic abscess can be single, multiple, or multiloculated.”
Diagnosis and treatment of focal splenic lesions
B. Malgras, H. Najah, A. Dohan et al.,
Journal of Visceral Surgery, https://doi.org/10.1016/j.jviscsurg.2021.11.010 - "On imaging, splenic candidiasis presents as multiple focal lesions that are small (< 1 cm) and rounded. They are hypoechoic on US, and minimally enhanced on CT and MRI. They are best visualized as hyper-intense on T2-weighted sequences and on diffusion sequences. Splenic candidiasis is most often associated with hepatic candidiasis, with hepatic lesions that show the same characteristics as the splenic lesions on imaging. MRI is suggestive when it reveals the ‘‘bull’s eye’’ sign (echogenic center sur- rounded by a hypo-echoic zone).”
Diagnosis and treatment of focal splenic lesions
B. Malgras, H. Najah, A. Dohan et al.,
Journal of Visceral Surgery, https://doi.org/10.1016/j.jviscsurg.2021.11.010 - “Sarcoidosis can affect all organs of the body; its manifesta- tions are non-specific, with clinical repercussions involving mainly the lungs, abdomen (pain) or systemic symptoms (fever, fatigue, weight loss). Imaging reveals splenic involve- ment in 6 to 33% of patients with sarcoidosis, although the prevalence of splenic involvement is between 24 and 59% when systematic histological analysis is performed, or even 38 to 77% in autopsy series. Splenic sarcoidosis is generally manifested by homogeneous splenomegaly that is present in approximately 40% of patients and much more rarely by focal splenic lesions.”
Diagnosis and treatment of focal splenic lesions
B. Malgras, H. Najah, A. Dohan et al.,
Journal of Visceral Surgery, https://doi.org/10.1016/j.jviscsurg.2021.11.010 - “When focal splenic lesions exist, they are often multi- ple, small in size (between 1 mm and 3 cm). They are rarely visible on US, and when they are, they are mildly hyperechoic. On CT, these lesions are mostly hypodense and contain small calcifications in 16% of cases. After IV contrast injection, the lesions are hypodense compared to the splenic parenchyma without peripheral enhancement. On MRI, the focal splenic lesions of sarcoidosis are hypo-intense with weak and late enhancement. They are better visible in T2-weighting with fat saturation, or in the early phase after injection. The lesional architecture is similar to that of lymphomas or splenic metastases.”
Diagnosis and treatment of focal splenic lesions
B. Malgras, H. Najah, A. Dohan et al.,
Journal of Visceral Surgery, https://doi.org/10.1016/j.jviscsurg.2021.11.010
