Imaging Pearls ❯ Practice Management ❯ Contrast Issues
|
-- OR -- |
|
- Sickle-Cell Trait/Disease: Some have suggested that contrast medium exposure to patients with sickle cell trait or sickle cell disease might increase the risk of an acute sickle crisis; however, there is no evidence this occurs with modern iodinated or gadolinium-based contrast medium. Therefore, restricting contrast medium use or premedicating solely on the basis of sickle cell trait or sickle cell disease is not recommended.
ACR Manual on Contrast Media 2023 - Patients premedicated for a prior contrast reaction have a breakthrough reaction rate (2.1%) that is 3-4 times the ordinary reaction rate in the general population, while patients premedicated for other indications have a breakthrough reaction rate close to 0%. In most cases (~81%), breakthrough reaction severity is similar to index reaction severity. Patients with a mild index reaction have a very low risk (<1%) of developing a severe breakthrough reaction.
ACR Manual on Contrast Media 2023 - Elective Premedication (12- or 13-hour oral premedication)
1. Prednisone-based: 50 mg prednisone by mouth at 13 hours, 7 hours, and 1 hour before contrast medium administration, plus 50 mg diphenhydramine intravenously, intramuscularly, or by mouth 1 hour before contrast medium administration [22]. Or
2. Methylprednisolone-based: 32 mg methylprednisolone by mouth 12 hours and 2 hours before contrast medium administration. 50 mg diphenhydramine may be added as in option 1 [39].
Although never formally compared, both regimens are considered similarly effective. The presence of diphenhydramine in regimen 1 and not in regimen 2 is historical and not evidence-based. Therefore, diphenhydramine may be considered optional.
ACR Manual on Contrast Media 2023 - “In patients with a prior allergic-like or unknown-type contrast reaction to a known contrast medium, changing contrast media within the same class (e.g., one iodinated medium for another) may help reduce the likelihood of a subsequent contrast reaction. Some studies have shown that the effect size of switching contrast media actually may be greater than that of premedication alone, but combining premedication with a change in agent seems to have the greatest effect. Unfortunately, many patients do not know which specific agent they have reacted to in the past; they simply remember they had a reaction. In the future, through improved electronic medical records, routine linking of reactions to specific contrast media is likely to add value. In the current state, investigating which agent was responsible for one or more prior reactions often is not possible. ”
ACR Manual on Contrast Media 2023 - Extravasations and severe extravasation injuries are more common in patients who 1) are uncommunicative, 2) have altered circulation in the injected extremity, 3) have had radiation of the injected extremity, or 4) are injected in the hand, foot, or ankle.
• Extravasations are also more common in patients injected with more viscous contrast material [6, 8, 35].
• The risk of extravasation can be minimized by 1) using angiocatheters rather than butterfly needles, 2) performing meticulous intravenous catheter insertion technique (confirming intravenous location by aspirating blood through an inserted catheter and flushing the inserted catheter with a test injection), 3) and carefully securing an inserted catheter.
ACR Manual on Contrast Media 2023 - Outpatients who have suffered contrast media extravasation should be released from the radiology department only after an initial period of observation, provided the radiologist is satisfied that any signs and symptoms that were present initially have improved or that new symptoms have not developed during the observation period. Clear instructions should be given to the patient to seek additional medical care for severe pain, progressive pain, numbness or tingling, diminished range of motion (active or passive), skin ulceration, or other neurologic or circulatory symptoms. This is because initial symptoms of a serious compartment syndrome may be absent or relatively mild (such as limited to the development of focal paresthesia).
ACR Manual on Contrast Media 2023 - The incidence of delayed allergic-like reactions has been reported to range from 0.5% to 14% . A prospective study of 258 individuals receiving intravenous iohexol demonstrated a delayed reaction rate of 14.3% compared to 2.5% in a control group undergoing imaging without intravascular contrast material. In that same study, 26 of 37 delayed adverse reactions were cutaneous in nature. For several reasons (lack of awareness of such adverse events, usual practice patterns, relatively low frequency of serious outcomes), such reactions are often not brought to the attention of the radiologist. Delayed reactions are more common in patients treated with interleukin-2 (IL-2) therapy . There is some evidence that the iso-osmolar dimer iodixanol may have a slightly higher rate of delayed cutaneous adverse events when compared to other LOCM . A prospective study by Schild et al demonstrated an increased frequency of delayed cutaneous adverse events to nonionic dimeric contrast material compared to nonionic monomeric contrast material.
ACR Manual on Contrast Media 2023
- • Enteric contrast continues to play an important role in the imaging assessment of patients presenting to the emergency department, especially when combined with computed tomography in specific clinical situations to improve diagnostic accuracy.
• Enteric contrast is particularly helpful in assessing postoperative complications of abdominal surgeries such as anastomotic leaks and fistulas.
• Although not always administered routinely, enteric contrast can be useful to confirm bowel injuries in the setting of penetrating trauma. Enteric contrast can assist in the identification of the appendix in cases of suspected acute appendicitis. Enteric contrast is also effective at guiding operative versus nonoperative management of patients with small-bowel obstruction.
• Although enteric contrast is overall safe and well-tolerated, the benefits of using it should be weighed against potential risks to the patient, including the time required to administer enteric contrast potentially resulting in a delay in diagnosis.
The Use of Enteric Contrast in the Emergency Setting
Mohamed Z. Rajput et al.
Radiol Clin N Am 61 (2023) 37–51 - “Extravasation of enteric contrast has been identified as the most specific sign of an anastomotic leak. CT combined with enteric contrast provides the best diagnostic assessment for identifying the presence and location of a leak with excellent anatomic detail as well as showing additional important findings that may be otherwise clinically unsuspected. Knowledge of the type of surgery and anastomoses performed is critical before determining the appropriate method for administering enteric contrast. To evaluate suspected leaks from esophageal, gastric, or small-bowel anastomoses, including patients following bariatric surgery, enteric contrast is administered orally or via an enteric tube, followed by an appropriate delay before scanning to ensure contrast has reached the anastomotic site.”
The Use of Enteric Contrast in the Emergency Setting
Mohamed Z. Rajput et al.
Radiol Clin N Am 61 (2023) 37–51 - “CT with oral contrast has been shown to have a high negative predictive value similar to that of fluoroscopy, and shows even greater sensitivity than fluoroscopy, for diagnosing esophageal perforation. In contrast to luoroscopy, CT can also be used to evaluate for extra-esophageal abnormalities that may be contributing to the patient’s symptoms. Protocols vary by institution but typically include precontrast imaging, supine post-contrast imaging performed immediately after administration of enteric contrast orally or via gastric tube placed into the esophagus, and, if needed, prone postcontrast imaging.”
The Use of Enteric Contrast in the Emergency Setting
Mohamed Z. Rajput et al.
Radiol Clin N Am 61 (2023) 37–51 - “Enteric contrast can play an important role in the diagnosis and management of patients with smallbowel obstruction. Typically, enteric contrast is not initially administered to patients with suspected small-bowel obstruction before obtaining CT, as many of these patients are experiencing nausea and/or vomiting limiting any oral intake. In addition, positive intraluminal contrast may potentially obscure the bowel wall and imaging signs of ischemia on CT. Though if enteric contrast had been administered because small-bowel obstruction was not suspected, it may help delineate the transition point of an obstruction where intraluminal contrast abruptly stops.”
The Use of Enteric Contrast in the Emergency Setting
Mohamed Z. Rajput et al.
Radiol Clin N Am 61 (2023) 37–51 - “In conclusion, enteric contrast continues to play an important role in the imaging assessment of patients presenting to the emergency department.Although it may no longer be required to ensure diagnostic accuracy on a routine basis, enteric contrast remains valuable, particularly when used in a targeted fashion to address specific clinical questions on a case-by-case basis. Enteric contrast is safe and well-tolerated by most patients with a low risk of serious side effects. A recent survey revealed that most patients (89%) would prefer to drink oral contrast, even with only the slightest likelihood that this will improve diagnostic accuracy, rather than accepting a risk of a missed finding. Radiologists report increased diagnostic confidence and reader reliability in cases in which any type of enteric contrast is used for CT imaging. This can be particularly important in the emergency setting, where one encounters critical, life-threatening pathologies requiring confident and accurate diagnoses on a routine basis.”
The Use of Enteric Contrast in the Emergency Setting
Mohamed Z. Rajput et al.
Radiol Clin N Am 61 (2023) 37–51
- BACKGROUND. Extrinsic warming of iodinated CT contrast media to body temperature reduces viscosity and injection pressures. However, studies examining the effect of extrinsic warming on clinical adverse events are limited in number and provide conflict- ing results. Therefore, consensus practice recommendations have been sparse.
OBJECTIVE. The purpose of this study is to compare rates of extravasation, allergic and allergic like reactions, and physiologic reactions between iohexol 350 mg I/mL warmed to body temperature (37°C) versus this agent maintained at room temperature.
CONCLUSION. The data suggest that maintaining iohexol 350 at room temperature is noninferior to warming the agent to body temperature before injection.
CLINICAL IMPACT. The resources involved to prewarm iohexol 350 before injection may not be warranted.
Effect of Extrinsic Warming of Low-Osmolality CT Contrast Media (Iohexol 350) on Extravasations and Patient Reaction Rates: A Retrospective Study
Noor F. Basharat et al.
AJR 2022; 218:174–179 - Key Finding
- Among 3939 patients who underwent CT using iohexol 350 prewarmed to body temperature, adverse reaction rate was 0.28%, which was not significantly different (p = .69) from the reaction rate of 0.43% among 3933 patients who received iohexol 350 maintained at room temperature; further analyses showed noninferiority at 0.6% margin.
Importance
- The resources required to warm iohexol 350 to body temperature before injection for CT may not be warranted given the lack of observed practical benefit.
Effect of Extrinsic Warming of Low-Osmolality CT Contrast Media (Iohexol 350) on Extravasations and Patient Reaction Rates: A Retrospective Study
Noor F. Basharat et al.
AJR 2022; 218:174–179 - “This study compared the rate of adverse reactions between patients who received iohexol 350 that had been extrinsically warmed to body temperature and patients who received this agent maintained at room temperature. The two groups showed no significant difference in the overall adverse event rate, extravasation rate, or rate of allergic and allergic like reactions. No physiologic reaction occurred in either group. Our findings question the utility of prewarming contrast media, which can be a resource-intensive process.”
Effect of Extrinsic Warming of Low-Osmolality CT Contrast Media (Iohexol 350) on Extravasations and Patient Reaction Rates: A Retrospective Study
Noor F. Basharat et al.
AJR 2022; 218:174–179 - "Our study has additional limitations. First, we solely assessed adverse reaction rates. We did not explore any potential impact of extrinsic warming on other end points, such as image quality or patient comfort. In addition, the body temperature group had a higher percentage of male patients, whereas the room temperature group had a larger needle gauge. The latter factor may have contributed to a potential decrease in adverse reaction rates in the room temperature group. Additionally, we noted a higher percentage of patients in the room temperature group who underwent CTA, which may also have had an impact on the data.”
Effect of Extrinsic Warming of Low-Osmolality CT Contrast Media (Iohexol 350) on Extravasations and Patient Reaction Rates: A Retrospective Study
Noor F. Basharat et al.
AJR 2022; 218:174–179 - Purpose: To evaluate the incidence and risk factors of late adverse reactions (ARs) to non-ionic low-osmolar contrast media (LOCM).
Methods: The occurrence of late AR was monitored on day 1 and from day 7 to day 28 in all patients who received enhanced computed tomography using LOCM during a 5-week study period in a single tertiary hospital. Patients who experienced late AR were followed up for three years.
Conclusions: Late ARs to LOCM occurred mostly within one week. The use of premedication may be helpful in reducing the recurrence of late ARs.
Incidence and risk factors of late adverse reactions to low-osmolar contrast media: A prospective observational study of 10,540 exposures
Dong Yoon Kang et al.
European Journal of Radiology 146 (2022) 110101 - Results: Among the total 10,540 LOCM exposures, 315 ARs (3.0%) were reported; acute ARs occurred in 108 LOCM exposures (1.0%) and late ARs occurred in 207 LOCM exposures (2.0%) (90.9% within one week, 9.1% developed afterwards by day 20). Previous history of drug allergy (odds ratio [OR] = 4.59; 95% confidence interval [CI] 2.17–9.71) and allergic diseases (OR = 2.54; 95% CI 1.32–4.91) were risk factors of late ARs to LOCM. Although the recurrence rate was lowered with premedication from 8.5% to 1.7% (8/94 vs. 3/178; p = 0.016), LOCM change did not make difference compared to reuse of the culprit LOCM (2/38 vs. 9/234; p = 0.655). In patients with a history of late AR to LOCM, the risk of recurrent reactions decreased with longer time intervals between exposures (OR = 0.86; 95% CI: 0.77–0.97; p = 0.025) and with the use of antihistamine premedication (OR = 0.27; 95% CI: 0.06–0.99; p = 0.049.
Incidence and risk factors of late adverse reactions to low-osmolar contrast media: A prospective observational study of 10,540 exposures
Dong Yoon Kang et al.
European Journal of Radiology 146 (2022) 110101 - “A late AR is defined as an AR that occurs after one hour and up to one week following exposure to a contrast medium and has a peak incidence from 3 h to two days after exposure. Common symptoms of late ARs include allergic-like ARs (maculopapular rashes, erythema, swelling, pruritus) and non-allergic-like ARs (nausea, vomiting, headache, musculoskeletal pain, and fever). Unlike acute ARs which appear to be associated with histamine release, late ARs are caused by a T cell- mediated reaction. Although symptoms of late ARs are usually mild, they can rarely manifest as severe reactions such as Stevens- Johnson syndrome or toxic epidermal necrosis.”
Incidence and risk factors of late adverse reactions to low-osmolar contrast media: A prospective observational study of 10,540 exposures
Dong Yoon Kang et al.
European Journal of Radiology 146 (2022) 110101 - "In conclusion, the incidence of late ARs following LOCM exposure was twice that of acute ARs, and symptoms in most cases developed within one week. A history of drug allergy and other allergic diseases was a significant risk factor in the occurrence of late ARs. In patients with a history of AR to LOCM, the risk of recurrent reactions decreases with longer time intervals between exposures. Premedication with antihistamines may also be effective in reducing the recurrence of patients with late AR.”
Incidence and risk factors of late adverse reactions to low-osmolar contrast media: A prospective observational study of 10,540 exposures
Dong Yoon Kang et al.
European Journal of Radiology 146 (2022) 110101
- IV Contrast Agent Selection
- Volume of contrast
- Type of contrast (non-ionic vs iso-osmolar)
- Concentration of contrast (300 vs 350 vs 370)
- Injection rate (cc/sec)
- Phases of acquisition(s) - Adult and Pediatric Patients
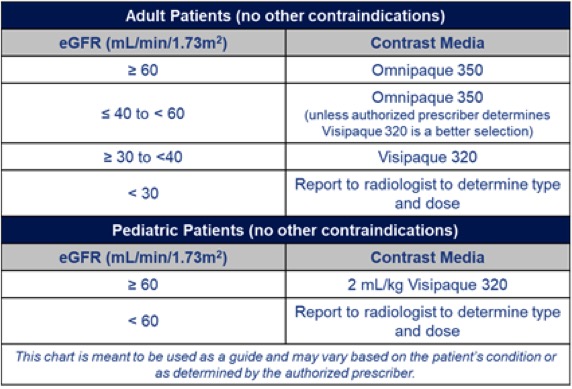
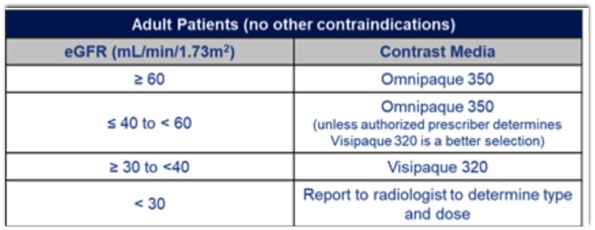
- Adult Patients
- Pediatric Patients
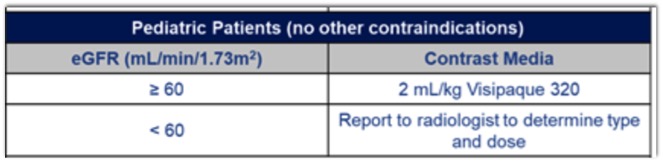
- Renal Function and Intravascular Iodinated Contrast Administration
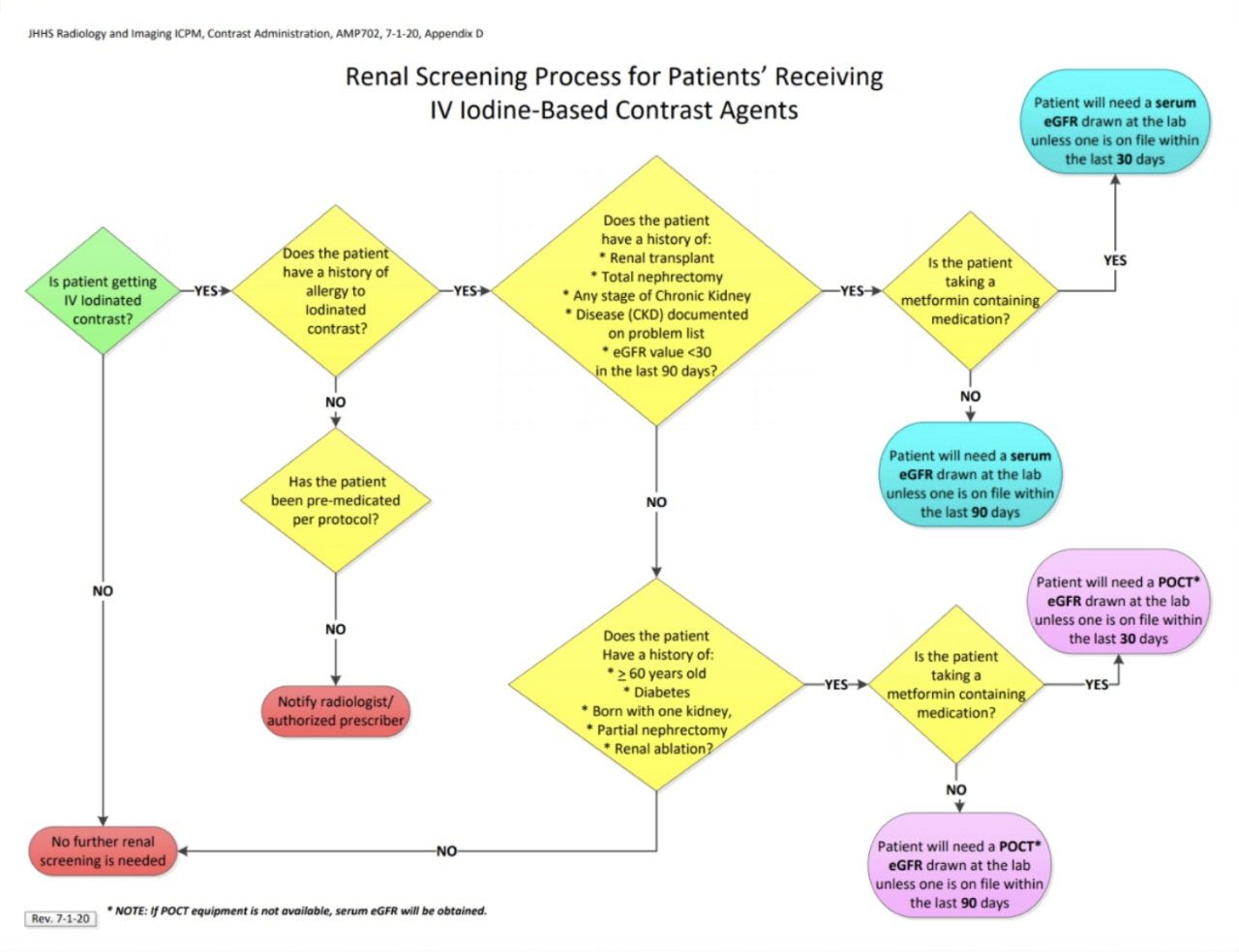
- Renal Function and Intravascular Iodinated Contrast Administration
- Dialysis Patients: Additional labs will not be needed as dialysis patients are already recognized to have an eGFR <30 mL/min/1.73m2 - Renal Function and Intravascular Iodinated Contrast Administration
- If the patient has any of the following risk factors and there is no eGFR value on record within 90 days, a serum creatinine/eGFR will be performed:
--- Renal transplantation
--- Total nephrectomy
--- Documentation of any stage of CKD in the EHR
--- Documentation of any eGFR value in the EHR within 90 days that is <30 mL/min/1.73m2 in patients who have no documented history of CKD or of currently being on dialysis - Renal Function and Intravascular Iodinated Contrast Administration
- If the patient has any of the following risk factors and there is no eGFR value on record within 90 days, a POCT creatinine/eGFR will be performed:
--- ≥ 60 years of age
--- Diabetes mellitus
--- Born with one kidney, partial nephrectomy, or renal ablation procedure - Renal Function and Intravascular Iodinated Contrast Administration
- If the patient is taking a metformin-containing medication:
--- Creatinine/eGFR values must be obtained within 30 days instead of 90 days.
--- POCT can be performed unless the patient has one of the risk factors identified requiring serum creatinine/eGFR. - Renal Function and Intravascular Iodinated Contrast Administration
- POCT creatinine/eGFR additional information:
--- If eGFR POCT is not available, serum eGFR will be obtained.
--- eGFR calculations should not be performed on the Nova StatSensor on patients under 18 years of age. Use approved eGFR calculator using the creatinine value obtained from the POCT meter.
--- POCT eGFR values will be documented in the electronic medical record.
- Should you place IV contrast in a warmer prior to using it?
- Yes
- No
- Not sure - Why would you not warm iodinated contrast?
- Cost and record keeping is needed
- Purchase warmer
- Keep log and monitor the warmer for correct temperature daily (Joint Commission rule)
- Need to label bottles with 30 day expiration date (Joint Commission rule) - “ Extrinsic warming (to 37° C) does not appear to affect adverse event rates for intravenous injections of iopamidol 300 of less than 6 ml/sec but is associated with a significant reduction in extravasation and overall adverse event rates for the more viscous iopamidol 370.”
Rate of Contrast Material Extravasations and Allergic-like Reactions: Effect of Extrinsic Warming of Low-Osmolality Iodinated CT Contrast Material to 37° C
Davenport MS et al.
Radiology 2012; 262:475-484
“Discontinuation of extrinsic warming (to 37° C) did not appear to affect adverse event rates for intravenous injections of iopamidol 300 of less than 6 ml/sec but was associated with an approximate tripling of extravasation and overall adverse event rates for the more viscous iopamidol 370.”
Rate of Contrast Material Extravasations and Allergic-like Reactions: Effect of Extrinsic Warming of Low-Osmolality Iodinated CT Contrast Material to 37° C
Davenport MS et al.
Radiology 2012; 262:475-484
