Imaging Pearls ❯ Pancreas ❯ Mucinous cystic neoplasm (MCN)
|
-- OR -- |
|
- Background: As pancreatic cystic neoplasms (PCN) differ in current standard of care, and these treatments can affect quality of life to varying degrees, a definitive preoperative diagnosis must be reliable. Current diagnostic approaches, specifically traditional cross- sectional imaging techniques, face certain limitations. But radiomics has been shown to have high diagnostic accuracy across a range of diseases. Objective to conduct a comprehensive review of the literature on the use of radiomics to differentiate Mucinous Cystic Neoplasm (MCN) from Serous Cystic Neoplasm (SCN). Methods: This study was comprehensively searched in Pubmed, Scopus and Web of Science databases for meta-analysis of studies that used radiomics to distinguish MCN from SCN. Risk of bias was assessed using the diagnostic accuracy study quality assessment method and combined with sensitivity, specificity, diagnostic odds ratio, and summary receiver operating characteristic (SROC)curve analysis.
Pancreatic Mucinous Cystic Neoplasm from Serous Cystic Neoplasm: Systematic Review and Meta-Analysis
Longjia Zhang1, Boyu Diao1, Zhiyao Fan1, Hanxiang Zhan, M.D, Ph.D
Acad Radiol 2025; 32:2679–2688 - Results: A total of 884 patients from 8 studies were included in this analysis, including 365 MCN and 519 SCN. The Meta-analysis found that radiomics identified MCN and SCN with high sensitivity and specificity, with combined sensitivity and specificity of 0.84(0.82–0.87) and 0.82(0.79–0.84). The positive likelihood ratio (PLR) and the negative likelihood ratio (NLR) are 5.61(3.72, 8.47) and 0.14(0.09–0.26). In addition, the area under the SROC curve (AUC) was drawn at 0.93. No significant risk of publication bias was detected through the funnel plot analysis. The performances of feature extraction from the volume of interest (VOI) or Using AI classifier in the radiomics models were superior to those of protocols employing region of interest (ROI) or absence of AI classifier. Conclusion: This meta-analysis demonstrates that radiomics exhibits high sensitivity and specificity in distinguishing between MCN and SCN, and has the potential to become a reliable diagnostic tool for their identification.
Pancreatic Mucinous Cystic Neoplasm from Serous Cystic Neoplasm: Systematic Review and Meta-Analysis
Longjia Zhang1, Boyu Diao1, Zhiyao Fan1, Hanxiang Zhan, M.D, Ph.D
Acad Radiol 2025; 32:2679–2688 - • The pooled sensitivity and specificity of radiomics for differentiating Mucinous Cystic Neoplasm from Serous Cystic Neoplasms were 84% and 82%, respectively.
• The field of radiomics lacks standardization, resulting in substantial variations in statistical analysis where such studies are conducted.
•Radiomics has an excellent diagnostic effect in distinguishing MCN from SCN and providing more critical information.
Pancreatic Mucinous Cystic Neoplasm from Serous Cystic Neoplasm: Systematic Review and Meta-Analysis
Longjia Zhang1, Boyu Diao1, Zhiyao Fan1, Hanxiang Zhan, M.D, Ph.D
Acad Radiol 2025; 32:2679–2688 - MCN is an uncommon tumor that usually occurs in middle-aged women. Surgery is the treatment of choice, and prognosis is excellent in the absence of invasive carcinoma (8). For SCN, the vast majority are benig. Studies have shown that most patients with SCN do not need surgery unless they have significant symptoms or a preoperative diagnosis is unclear. Therefore, some patients can choose to follow-up. Compared with SCN, MCN has considerable malignant potential, so the guidelines recommend resections for all patients who are suitable for surgery. Therefore, it is important to distinguish MCN from SCN in clinic, but current diagnostic approach (ie, traditional cross-sectional imaging) has limitations. It has been reported that the discrimination efficacy of CT for SCNs was ranged from 43% to 67%
Pancreatic Mucinous Cystic Neoplasm from Serous Cystic Neoplasm: Systematic Review and Meta-Analysis
Longjia Zhang1, Boyu Diao1, Zhiyao Fan1, Hanxiang Zhan, M.D, Ph.D
Acad Radiol 2025; 32:2679–2688 - “ Our study discovered that radiomics possesses a high degree of accuracy in distinguishing PCNs, particularly in detecting MCN and SCN, making it worthy of promotion for broader application. However, we require additional high-quality research to further validate these findings, and its practical efficiency and clinical applicability also need to be explored further. Moreover, we anticipate establishing standardized radiomics guidelines in the future to provide more evidence for the diagnosis and treatment of pancreatic cystic neoplasms.”
Pancreatic Mucinous Cystic Neoplasm from Serous Cystic Neoplasm: Systematic Review and Meta-Analysis
Longjia Zhang1, Boyu Diao1, Zhiyao Fan1, Hanxiang Zhan, M.D, Ph.D
Acad Radiol 2025; 32:2679–2688
- Background: Mucinous cystic neoplasms of the pancreas are uncommon tumors that have the potential of becoming cancer. There is no consensus regarding the high-risk features of these tumors. Our study aimed to identify the preoperative demographic, clinical, or radiologic factors that can predict the presence of high-grade dysplasia or invasive carcinoma in mucinous cystic neoplasms of the pancreas.
Conclusion: Tumors with a size 4 cm and/or a high CA 19-9 level should be considered for prompt surgical resection. Conversely, tumors <4 cm with no other high-risk features have a negligible risk for high-grade dysplasia or invasive carcinoma and may benefit from nonoperative surveillance. Mural nodularity is an additional suspicious feature. These findings may contribute to future guidelines.
Identification of high-risk features in mucinous cystic neoplasms of the pancreas
Maximiliano Servin-Rojas et al.
Surgery (2023) in press - Results: The rate of high-grade dysplasia or invasive carcinoma was 11%. Tumor size 4 cm (P < .001), mural nodularity (P . .04), and a serum CA 19-9 level >37 U/mL (P < .001) were associated with high grade dysplasia or invasive carcinoma. In the multivariable analysis, tumor size 4 cm (odds ratio 16.9, 95% confidence interval 2.04e140, P . .009) and a CA 19-9 level >37 U/mL (odds ratio 5.68, 95% confidence interval 1.52e21.3, P ..010) were predictors of high-grade dysplasia or invasive carcinoma. There were no tumors with high-grade dysplasia or invasive carcinoma in patients with tumor size <4 cm in the absence of an elevated CA 19-9 or mural nodularity.
Identification of high-risk features in mucinous cystic neoplasms of the pancreas
Maximiliano Servin-Rojas et al.
Surgery (2023) in press - “In conclusion, in our study, the rate of HGD/IC among patients with a pathologically confirmed diagnosis of MCNs was 11%, which is similar to prior series. Tumor size 4 cm and elevated serum CA 19-9 were significant predictors of HGD/IC in our study. Specifically, tumor size <4 cm could reliably exclude HGD/IC, especially in the absence of other associated high-risk features, such as elevated CA 19-9 or the presence of mural nodularity. These findings appear to distinguish which patients with pancreatic MCNs may benefit from surgical resection versus those who can be spared an operation and associated complications.”
Identification of high-risk features in mucinous cystic neoplasms of the pancreas
Maximiliano Servin-Rojas et al.
Surgery (2023) in press
- “Results: Twenty-five (78%) patients presented with symptoms and 8 (25%) patients had abnormal serum biochemical values. Mean MCN maximum dimensions were 48 9 45 9 45 mm with a mean volume of 169 mL. MCN were located in the tail (n = 18), body (n = 10), neck (n = 2), and (head = 2); 30 (93.5%) MCN were encapsulated, 3 (9%) had calcifications, 4 (12%) showed enhancing nodules, 9 (28%) had enhancing septations, and 5 (15%) had main pancreatic duct dilation. Associated chronic pancreatitis was observed in 4 (12%) patients. The only predictors for high-grade dysplasia/carcinoma were MCN size and volume. Using a cut-off size greater than 8.5 cm, the specificity and sensitivity for high-grade dysplasia/carcinoma were 97 and 60%, respectively (p = 0.003; OR 81, 95% CI 3.9–1655.8). Mean MCN growth rate was estimated at 4.2 mm/year with a doubling time of 8.23 years.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - "MCN size (> 8.5 cm) and volume are the only features on MDCT/MR imaging that correlate with high-grade dysplasia/carcinoma. The average growth rate for MCNs is slow at approximately 4 mm per year.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - "Mucinous cystic neoplasms (MCN) of the pancreas are uncommon tumors that are nearly exclusively seen in middle-aged females. Although the vast majority of MCN are benign at time of diagnosis, they are considered pre-malignant lesions that may become dysplastic and malignant over time. To the best of our knowledge, the exact timeline for this progression is unknown. Needless to say, the ability to predict non-invasively the pathological subtype of MCN can have important advantages and implications. Firstly, biopsy of MCN is prone to sample bias as the epithelial lining of the cyst may be normal in one location but dysplastic or frankly malignant in others. Secondly, MCN with low-grade dysplasia may be treated conservatively with observation rather than surgery, especially in elderly patients with co- morbidities. Lastly, indications for high-grade dysplasia or carcinoma may trigger immediate surgical resection.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - “In our series, all patients were women with a mean age of 45 years. Indeed, MCN is referred to as the ‘mother cyst’ and the previously reported distribution of MCN by gender is 89–99.7% female with a reported mean age at time of diagnosis of 48 years (range, 17–78 years). Presenting clinical signs and symptoms along with serologic biochemical values were also evaluated and correlated with pathology. Although in our cohort 75% of patients presented with at least one symptom, we did not identify any correlation between clinical symptoma- tology with the presence of high-grade dysplasia/carci- noma.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - "In conclusion, MCN size (> 8.5 cm) and volume are the only features on MDCT/MR imaging that correlates with high-grade dysplasia/carcinoma. Moreover, no clinical symptoms, biochemical abnormalities, or pre-operative cyst features previously described as potential predictors high-grade dysplasia/carcinoma could be reproduced. The average growth rate for MCNs is slow at approximately 4 mm per year.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - “Mucinous cystic neoplasms (MCN) of the pancreas are rare, low-grade tumors that occur predominantly in middle-aged women . They are reported to be maligant in about 6–27% of cases. Their most characteristic histopathological finding is the combination of mucin-producing epithelium supported by characteristic ovarian-like stroma that is not found in other pancreatic neoplasms. Furthermore, they usually are com- posed of large (> 2 cm) unilocular or multilocular macrocysts devoid of communication between the cyst and the pancreatic ductal system, and the presence of a fibrous capsule. All MCNs have the potential to transform into an invasive carcinoma, hence the necessity to resect them in their totality.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422
- Pancreatic Cysts on CT: Potentially or Definitely Malignant
- Intraductal Papillary Mucinous Neoplasm
- Mucinous Cystic Neoplasm - Pancreatic Cysts on CT: Definitely Malignant Cystic Lesions
- Solid and Pseudopapillary Epithelial Neoplasms (SPEN)
- Cystic Features of Pancreatic Ductal Adenocarcinoma
- Cystic Neuroendocrine Tumor - "SCNs typically are described as having a honeycomb or multilocular appearance with or without a central scar. However, there can be variations in the morphologic appearance with polycystic, oligocystic, and solid patterns described. Microcystic morphology is more common in SCNs. The classic imaging features are a lobulated external contour and central scar with stellate calcification. SCNs rarely demonstrate peripheral enhancing capsule or mural nodules.”
Incidental Pancreatic Cysts on Cross-Sectional Imaging
Shannon M. Navarro et al.
Radiol Clin N Am 59 (2021) 617–629 - "IPMNs are cystic neoplasms with variable degree of malignant potential. They may evolve into dysplasia or invasive carcinoma and are associated with a higher risk for the development of PDAC in the gland separate from the IPMN sites. The rate of progression increases with time. Low-risk IPMNs have an approximately 8% chance of progression, whereas higher risk IPMNs have an approximately 25% chance of progression to PDAC in 10 years. Even presumed low- risk BD-IPMNs may demonstrate growth after 5 years.”
Incidental Pancreatic Cysts on Cross-Sectional Imaging
Shannon M. Navarro et al.
Radiol Clin N Am 59 (2021) 617–629 - "MCNs occur almost exclusively in women and more commonly are found in the pancreatic tail. MCNs are oval or round and can show septations, cyst wall calcifications, enhancing capsules, and occasionally mural nodules. MCNs typically do not cause dilatation of the biliary or pancreatic ductal system but can be associated with distal pancreatic atrophy. They may be associated with lymphadenopathy but generally are not associated with peripancreatic fat infiltration or vascular involvement.”
Incidental Pancreatic Cysts on Cross-Sectional Imaging
Shannon M. Navarro et al.
Radiol Clin N Am 59 (2021) 617–629 - "Incidental PCs commonly are encountered in a radiology practice. Some cystic masses of the pancreas, in particular pseudocysts, usually can be characterized accurately and adequately by a combination of imaging, history, and follow-up. Other PCs require further evaluation with EUS with FNA. Because some have malignant potential, many PCs require clinical and imaging follow-up. There are several available societal guidelines to help plan patient follow-up, with recent updates. The care of patients with PCs ideally is a multidisciplinary effort among radiologists, pathologists, surgeons, and gastroenterologists for optimal patient management.”
Incidental Pancreatic Cysts on Cross-Sectional Imaging
Shannon M. Navarro et al.
Radiol Clin N Am 59 (2021) 617–629 - • Imaging alone cannot always differentiate benign pancreatic cysts from pancreatic cysts with malignant potential.
• Small indeterminate pancreatic cysts need to be followed-up, since invasive testing and resections are typically reserved for larger or growing cysts or definitively malignant cysts.
Incidental Pancreatic Cysts on Cross-Sectional Imaging
Shannon M. Navarro et al.
Radiol Clin N Am 59 (2021) 617–629
- “MCNs occur almost exclusively in women and more commonly are found in the pancreatic tail. MCNs are oval or round and can show septations, cyst wall calcifications, enhancing capsules, and occasionally mural nodules. MCNs typically do not cause dilatation of the biliary or pancreatic ductal system but can be associated with distal pancreatic atrophy. They may be associated with lymphadenopathy but generally are not associated with peripancreatic fat infiltration or vascular involvement.”
Incidental Pancreatic Cysts on Cross-Sectional Imaging
Shannon M. Navarro et al.
Radiol Clin N Am 59 (2021) 617–629 - Cystic Pancreatic Lesions
- Pancreatic Pseudocyst
- Serous cystadenoma
- Lymphoepithelial Cyst
- IPMN
- MCN (Mucinous Cystic Neoplasm)
- Solid and Pseudopapillary Epithelial Neoplasms (SPEN)
- Cystic Features of Pancreatic Ductal Adenocarcinoma
- Cystic Neuroendocrine Tumor - “Predictors of high-grade dysplasia (MCN) include size greater 8.5 cm.”
Incidental Pancreatic Cysts on Cross-Sectional Imaging
Shannon M. Navarro et al.
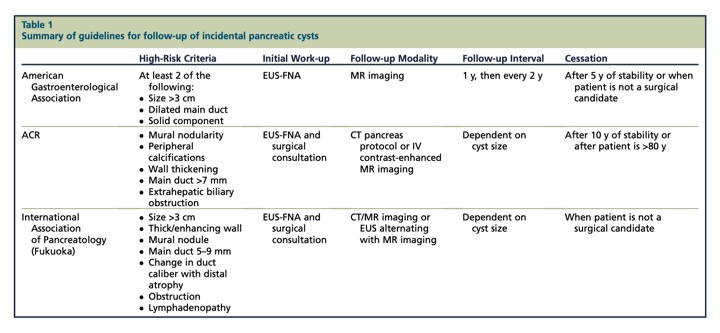
Radiol Clin N Am 59 (2021) 617–629 - Summary of guidelines for follow-up of incidental pancreatic cysts
- MCN vs SCN using EUS
- “Mucinous cystic neoplasms (MCN) and serous cystic neoplasms (SCN) account for a large portion of solitary pancreatic cystic neoplasms (PCN). In this study we implemented a convolutional neural network (CNN) model using ResNet50 to differentiate between MCN and SCN. The training data were collected retrospectively from 59 MCN and 49 SCN patients from two different hospitals. Data augmentation was used to enhance the size and quality of training datasets. Fine-tuning training approaches were utilized by adopting the pre-trained model from transfer learning while training selected layers. Testing of the network was conducted by varying the endoscopic ultrasonography (EUS) image sizes and positions to evaluate the network performance for differentiation. The proposed network model achieved up to 82.75% accuracy and a 0.88 (95% CI: 0.817–0.930) area under curve (AUC) score.”
Deep Learning-Based Differentiation between Mucinous Cystic Neoplasm and Serous Cystic Neoplasm in the Pancreas Using Endoscopic Ultrasonography
Leang Sim Nguon et al.
Diagnostics 2021, 11, 1052. https://doi.org/10.3390/diagnostics11061052 - “Results: Twenty-five (78%) patients presented with symptoms and 8 (25%) patients had abnormal serum biochemical values. Mean MCN maximum dimensions were 48 9 45 9 45 mm with a mean volume of 169 mL. MCN were located in the tail (n = 18), body (n = 10), neck (n = 2), and (head = 2); 30 (93.5%) MCN were encapsulated, 3 (9%) had calcifications, 4 (12%) showed enhancing nodules, 9 (28%) had enhancing septations, and 5 (15%) had main pancreatic duct dilation. Associated chronic pancreatitis was observed in 4 (12%) patients. The only predictors for high-grade dysplasia/carcinoma were MCN size and volume. Using a cut-off size greater than 8.5 cm, the specificity and sensitivity for high-grade dysplasia/carcinoma were 97 and 60%, respectively (p = 0.003; OR 81, 95% CI 3.9–1655.8). Mean MCN growth rate was estimated at 4.2 mm/year with a doubling time of 8.23 years.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - "MCN size (> 8.5 cm) and volume are the only features on MDCT/MR imaging that correlate with high-grade dysplasia/carcinoma. The average growth rate for MCNs is slow at approximately 4 mm per year.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - "Mucinous cystic neoplasms (MCN) of the pancreas are uncommon tumors that are nearly exclusively seen in middle-aged females. Although the vast majority of MCN are benign at time of diagnosis, they are considered pre-malignant lesions that may become dysplastic and malignant over time. To the best of our knowledge, the exact timeline for this progression is unknown. Needless to say, the ability to predict non-invasively the pathological subtype of MCN can have important advantages and implications. Firstly, biopsy of MCN is prone to sample bias as the epithelial lining of the cyst may be normal in one location but dysplastic or frankly malignant in others. Secondly, MCN with low-grade dysplasia may be treated conservatively with observation rather than surgery, especially in elderly patients with co- morbidities. Lastly, indications for high-grade dysplasia or carcinoma may trigger immediate surgical resection.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - “In our series, all patients were women with a mean age of 45 years. Indeed, MCN is referred to as the ‘mother cyst’ and the previously reported distribution of MCN by gender is 89–99.7% female with a reported mean age at time of diagnosis of 48 years (range, 17–78 years). Presenting clinical signs and symptoms along with serologic biochemical values were also evaluated and correlated with pathology. Although in our cohort 75% of patients presented with at least one symptom, we did not identify any correlation between clinical symptoma- tology with the presence of high-grade dysplasia/carci- noma.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - "In conclusion, MCN size (> 8.5 cm) and volume are the only features on MDCT/MR imaging that correlates with high-grade dysplasia/carcinoma. Moreover, no clinical symptoms, biochemical abnormalities, or pre-operative cyst features previously described as potential predictors high-grade dysplasia/carcinoma could be reproduced. The average growth rate for MCNs is slow at approximately 4 mm per year.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422 - “Mucinous cystic neoplasms (MCN) of the pancreas are rare, low-grade tumors that occur predominantly in middle-aged women . They are reported to be maligant in about 6–27% of cases. Their most characteristic histopathological finding is the combination of mucin-producing epithelium supported by characteristic ovarian-like stroma that is not found in other pancreatic neoplasms. Furthermore, they usually are com- posed of large (> 2 cm) unilocular or multilocular macrocysts devoid of communication between the cyst and the pancreatic ductal system, and the presence of a fibrous capsule. All MCNs have the potential to transform into an invasive carcinoma, hence the necessity to resect them in their totality.”
Mucinous cystic neoplasms of the pancreas: high-resolution cross-sectional imaging features with clinico-pathologic correlation
Alejandro Garces-Descovich et al.
Abdom Radiol (2018) 43:1413–1422
- “Mucous producing neoplasms are classified into intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms (MCNs), which have distinct biological characteristics. IPMNs arise in the main pancreatic duct or its major branches, whereas MCNs are large cysts with a thick, peripheral rim of calcifications that do not communicate with the pancreatic ductal system.”
Pancreatic mucinous cystadenocarcinoma: Epidemiology and outcomes Doulamis, Ilias P. et al. International Journal of Surgery , Volume 35 , 76 - 82 - “MCACs are usually symptomatic at the time of diagnosis, with obstructive jaundice and palpable abdominal mass being commonly present (>25%). Notably, portal hypertension, hemobilia and diabetes mellitus constitute signs of aggressive malignancy. Apart from clinical presentation and imaging techniques, cyst fluid analysis may be useful in the preoperative differential diagnosis of these patients, since detecting K-RAS mutations, carcinoembryonic antigen levels >400 ng/ml and CA19-9 >50,000 U/ml may indicate malignancy over a benign lesion, such as a pseudocyst.”
Pancreatic mucinous cystadenocarcinoma: Epidemiology and outcomes Doulamis, Ilias P. et al. International Journal of Surgery , Volume 35 , 76 - 82 - ” In the present study, median patient age at diagnosis was 67 years and the majority was white females. Findings from literature review indicated a similar age range (29–89 years), but over a decade younger with a mean age of 54.3 years. Only two studies reported data regarding patient race; in both studies white race dominated (87.6%). It should be noted that, before 2000, small case-series advocated that female predominance is less common in pancreatic mucinous cystadenocarcinoma compared with benign cystic tumors and some studies even found higher prevalence in males.”
Pancreatic mucinous cystadenocarcinoma: Epidemiology and outcomes Doulamis, Ilias P. et al. International Journal of Surgery , Volume 35 , 76 - 82 - ” In the present study, median patient age at diagnosis was 67 years and the majority was white females. Findings from literature review indicated a similar age range (29–89 years), but over a decade younger with a mean age of 54.3 years. Only two studies reported data regarding patient race; in both studies white race dominated (87.6%). It should be noted that, before 2000, small case-series advocated that female predominance is less common in pancreatic mucinous cystadenocarcinoma compared with benign cystic tumors and some studies even found higher prevalence in males .With regard to tumor location, body/tail were the most frequently affected sites both in the SEER analysis (45.6%) and in accordance to literature, despite outdated reports implicating the head of the pancreas as the most common MCAC site.”
Pancreatic mucinous cystadenocarcinoma: Epidemiology and outcomes Doulamis, Ilias P. et al. International Journal of Surgery , Volume 35 , 76 - 82 - ” All in all, the prognosis of resectable MCAC seems to be significantly more favorable compared to pancreatic ductal adenocarcinoma, and inoperability is associated with very poor outcomes. To the best of our knowledge this is the largest population-based study specifically dedicated to the epidemiology and outcomes of patients with pancreatic mucinous cystadenocarcinomas. The major strength of our study is that it limits publication bias, which traditionally hinders the applicability of results generated by secondary research papers. It should be noted that 66.7% of the SEER cases were diagnosed after 2000, whereas most of the studies identified were published before 2000 and mainly consisted of small case series (11–78 patients).”
Pancreatic mucinous cystadenocarcinoma: Epidemiology and outcomes Doulamis, Ilias P. et al. International Journal of Surgery , Volume 35 , 76 - 82
