Imaging Pearls ❯ GU Misc ❯ Retroperitoneal Sarcoma
|
-- OR -- |
|
- "Primary retroperitoneal masses, which originate in the retroperitoneum but outside the major retroperitoneal organs, are uncommon and can be divided primarily into solid and cystic masses, each of which can be further subdivided into neoplastic and nonneoplastic masses .Of the primary retroperitoneal neoplasms, 70%–80% are malignant in nature, and these account for 0.1%–0.2% of all malignancies in the body."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
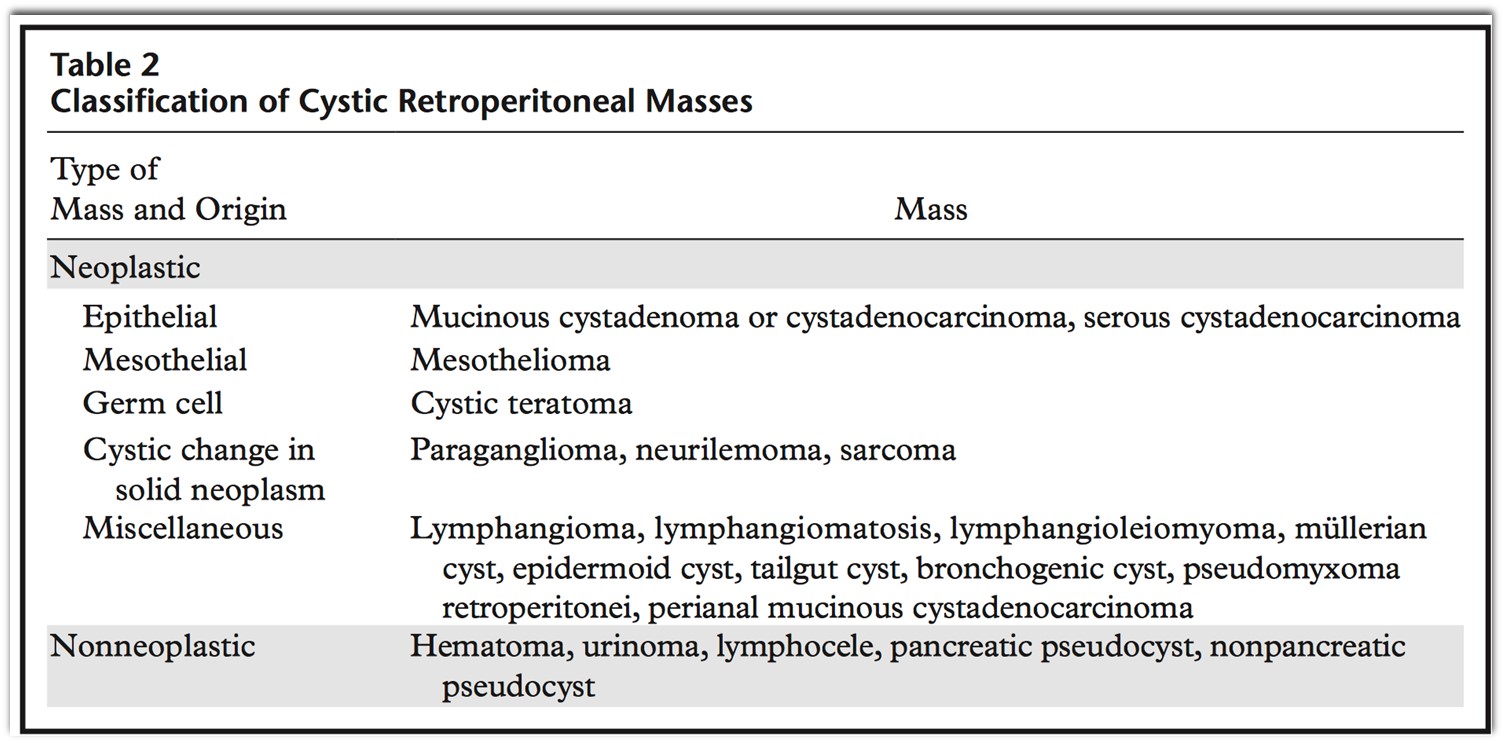
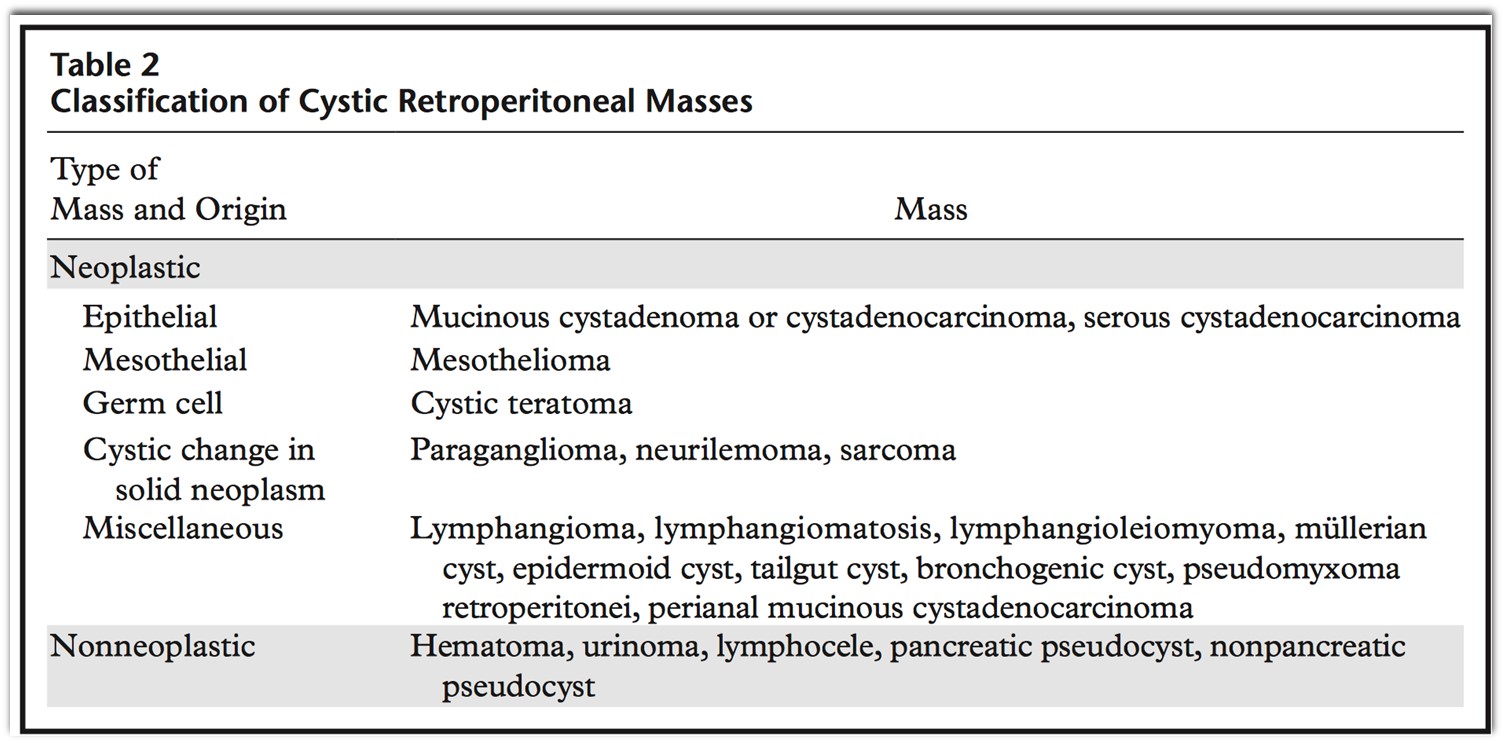
RadioGraphics 2011; 31:949–976 - Cystic Retroperitoneal Masses
- "Solid neoplasms in the retroperitoneum can be broadly divided into four groups: (a) mesodermal neoplasms; (b) neurogenic tumors; (c) germ cell, sex cord, and stromal tumors; and (d) lym- phoid and hematologic neoplasms."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Retroperitoneal sarcomas constitute 0.1%–0.2% of all malignancies. Most of the retroperitoneal neoplasms are of mesodermal origin, with
liposarcomas, leiomyosarcomas, and malignant fibrous histiocytomas making up more than 80% of these tumors. Retroperitoneal sarcomas are commonly seen in the 5th and 6th decades of life. These tumors are large at the time of clinical pre- sentation and often involve adjacent structures. Compression of adjacent organs causes formation of a pseudocapsule.The recurrence rates are high, and metastases to liver, lung, bones, and brain may be seen."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Liposarcoma is the most common (33%) primary retroperitoneal sarcoma. Ten to fifteen percent of liposarcomas occur in the retroperitoneum, and they are more common in the 50–70-year age group, with no sex predilection. Histologically, liposarcoma is classified, in increasing order of malignancy, into four subtypes: well-differentiated, myxoid, pleomorphic, and round cell subtypes. Various histologic subtypes may be seen in the same lesion. Liposarcoma is usually large (average diameter, >20 cm) and is a slow-growing tumor."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "The well-differentiated subtype, the most common type of retroperitoneal liposarcoma, is a predominantly hypoattenuating lesion on CT images because of its fat content."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Leiomyosarcoma is the second most common (28%) primary retroperitoneal sarcoma. Leiomyosarcoma arises from retroperitoneal smooth muscle tissue, blood vessels, or wolf an duct remnants and can grow to a large size (>10 cm) before compromising adjacent organs and precipitating clinical symptoms such as venous thrombosis. Leiomyosarcoma is more common in women, in the 5th to 6th decades of life."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Approximately 6% of leiomyosarcomas arise from the IVC. Most of these tumors have a large extravascular component that makes it difficult to distinguish them from a secondary involvement of the IVC with an extrinsic tumor.The most commonly affected location is the segment between the diaphragm and renal veins."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "At CT, leiomyosarcoma of the IVC is depicted as an intermediate- attenuation mass with heterogeneous enhance- ment. Intraluminal masses result in expansion and obstruction of the IVC, and extraluminal masses cause extrinsic compression and proximal dilation."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Neurogenic tumors constitute 10%–20% of primary retroperitoneal tumors. Compared with the mesenchymal tumors, neurogenic tumors occur in a younger age group and are more likely to be benign and have a better prognosis. Neurogenic tumors can originate from the nerve sheath (schwannoma, neuro broma, neurofibromatosis, malignant nerve sheath tumors), ganglionic cells (ganglioneuroma, ganglioneuroblastoma, neuroblastoma), or paraganglionic cells (paraganglioma, pheochromocytoma)."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Neurogenic tumors are seen commonly (a) along the sympathetic ganglia, which are located in the paraspinal region, and (b) in the adrenal medulla or the organs of Zuckerkandl (paraaortic bodies). Less commonly, neurogenic tumors occur in other sites, such as the urinary bladder, abdominal wall, bowel wall, or gallbladder."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Schwannoma, or neurilemoma, is a benign tumor that arises from the perineural sheath of Schwann (neurilemma). Schwannoma accounts for 6% of retroperitoneal neoplasms and is more common than neurofibroma. Schwannoma is usually asymptomatic and is more common in females (2:1), particularly in the 20–50-year age group."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "At CT, small schwannomas are round, well defined, and homogeneous, but large schwannomas may be heterogeneous in appearance. Calcification can be punctate, mottled, or curvilinear. The nerve of origin is often difficult to identify. After contrast enhancement, schwannoma demonstrates variable homogeneous or heterogeneous enhancement."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Neurofibroma is a benign nerve sheath tumor that can occur as an isolated tumor (90%) or as part of type 1 neuro fibromatosis. Approximately 30% of solitary tumors and 100% of multiple tumors or plexiform neurofibromas are associated with type 1 neurofibromatosis. Neuro- fibroma is more common in men, particularly in the 20–40-year age group."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "At CT, neurofibroma is depicted as a well- defined round homogeneously hypoattenuating lesion (20–25 HU) because of the presence of lipid-rich Schwann cells and adipocytes and en- trapment of adjacent fat. Typically, there is homogeneous contrast enhancement (30–50 HU) that is due to collagen bands, but cystic areas caused by myxoid degeneration may be seen."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Ganglioneuroma is a rare benign tumor that arises from the sympathetic ganglia. It is usually asymptomatic but can manifest with pain or a mass. Ganglioneuroma occasionally secretes hormones such as catecholamines, vasoactive intestinal peptides, or androgenic hormones.This tumor is commonly seen in the 20–40- year age group, with no sex predilection . Histopathologically, ganglioneuroma is composed of Schwann cells, ganglion cells, and nerve fibers."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Teratoma is a germ cell tumor that originates from pluripotent germ cells that have been interrupted in their normal migration to the genital ridges. Less than 10% of teratomas are found in the retroperitoneum. Teratoma accounts for as many as 11% of primary retroperitoneal tumors and is the third most common tumor in the retroperitoneum in children, after neuroblastoma and Wilms tumor."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Teratoma is more common in females, with a bimodal age distribu- tion (<6 months and early adulthood). Teratoma can be benign or malignant, and benign teratoma can be either mature or immature."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Mature teratoma (dermoid cyst) contains well- differentiated tissues from at least two germ cell layers. Ectodermal layers are seen in all, mesodermal layers in 90% of lesions, and endodermal layers in the majority of lesions. Mature teratomas are predominantly cystic. Calcification (toothlike or well defined) and fat can be seen in 56% and 93% of cases, respectively."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "A fat-fluid (sebum) level and chemical shift between fat and fluid are pathognomonic. A villiform solid component known as a Rokitansky protuberance is seen in 81% of cases. Malignancy has been reported in 2%–3% of mature teratomas, more commonly in children (26%) than adults (10%), and is associated with wall thickening, irregular margins, and infiltration of adjacent organs."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Compared with mature teratoma, immature teratoma is less common (<1%), contains more than 10% undifferentiated tissue, and is seen in
a younger age group (<20 years). The most common location of immature teratoma is near the upper pole of the left kidney. Immature tera- toma is predominantly solid, with scattered areas of fat and calcification (coarse and ill de fined), but cystic components are found occasionally."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976 - "Malignant teratoma can have germ cell or non–germ cell malignant tissue. Malignant trans- formation is less common in the retroperitoneum (38). Malignant tumors are irregular, with inva- sion of adjacent structures and vascular invasion. A poor prognosis is associated with lesions with germ cells or lesions with rhabdomyosarcoma or neural differentiation. An elevated a-fetoprotein level is found in 50% of malignant teratomas. Surgical resection is required for definitive diagnosis and treatment."
Imaging of Uncommon Retroperitoneal Masses
Rajiah P et al.
RadioGraphics 2011; 31:949–976