Imaging Pearls ❯ November 2014
|
-- OR -- |
|
Chest
- NCI Factsheet
- Tobacco smoke is harmful to smokers and nonsmokers.
- Cigarette smoking causes many types of cancer, including cancers of the lung, esophagus, larynx (voice box), mouth, throat, kidney, bladder, pancreas, stomach, and cervix, as well as acute myeloid leukemia.
- Quitting smoking reduces the health risks caused by exposure to tobacco smoke. - “The purpose of this study was to review the records of patients with diagnoses of lung cancer in annual repeat rounds of CT screening in the International Early Lung Cancer Action Program to determine whether the cancer could have been identified in the previous round of screening.”
Retrospective Review of Lung Cancers Diagnosed in Annual Rounds of CT Screening
Xu DM et al.
AJR Am J Roentgenol. 2014 Sep 23:1-8 - “Three radiologists reviewed the scans of 104 lung cancer patients and assigned the findings to one of three categories: 1, cancer was not visible at previous CT screening; 2, cancer was visible at previous CT screening but not identified; 3, abnormality was identified at previous CT screening but not classified as malignant. Nodule size, nodule consistency, cell type, and stage at the previous screening and when identified for further workup for each of the three categories were tabulated.”
Retrospective Review of Lung Cancers Diagnosed in Annual Rounds of CT Screening
Xu DM et al.
AJR Am J Roentgenol. 2014 Sep 23:1-8 - “Three radiologists reviewed the scans of 104 lung cancer patients and assigned the findings to one of three categories:
1, cancer was not visible at previous CT screening;
2, cancer was visible at previous CT screening but not identified;
3, abnormality was identified at previous CT screening but not classified as malignant.”
Retrospective Review of Lung Cancers Diagnosed in Annual Rounds of CT Screening
Xu DM et al.
AJR Am J Roentgenol. 2014 Sep 23:1-8 - “Twenty-four (23%) patients had category 1 findings; 56 (54%) category 2; and 24 (23%) category 3. When diagnosed, seven (29%) category 1, 10 (18%) category 2, and four (17%) category three cancers had progressed beyond stage I. All cancers seen in retrospect were in clinical stage I at the previous screening. Category 1 cancers, compared with categories 2 and 3, had faster growth rates, were less frequently adenocarcinomas (29% vs 54% and 67%, p = 0.01), and were more often small cell carcinomas (29% vs 14% and 12%, p = 0.12).”
Retrospective Review of Lung Cancers Diagnosed in Annual Rounds of CT Screening
Xu DM et al.
AJR Am J Roentgenol. 2014 Sep 23:1-8 - “ Lung cancers found on annual repeat screenings were frequently identified in the previous round of screening, suggesting that review of the varied appearance and incorporation of advanced image display may be useful for earlier detection. ”
Retrospective Review of Lung Cancers Diagnosed in Annual Rounds of CT Screening
Xu DM et al.
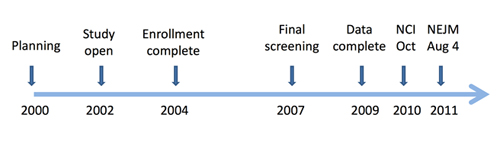
AJR Am J Roentgenol. 2014 Sep 23:1-8 - “ In lung cancer, early detection and diagnosis is of paramount importance. In 2011 the National Lung Screening Trial (NLST) demonstrated the effectiveness of computed tomography (CT) screening for lung cancer in reducing mortality, and results from other ongoing trials are expected to be published in the near future. A topic that has not been widely researched to date, however, is the cause for screening failure and missed lung cancers. In this issue of European Radiology, Scholten et al. describe a number of causes for false-negative screens. Some of the implications for CT screening and nodule management raised by this report are discussed. “
Missed cancers in lung cancer screening - more than meets the eye
Devaraj A.
Eur Radiol. 2014 Sep 5. [Epub ahead of print] - “A topic that has not been widely researched to date, however, is the cause for screening failure and missed lung cancers. In this issue of European Radiology, Scholten et al. describe a number of causes for false-negative screens. Some of the implications for CT screening and nodule management raised by this report are discussed.”
Missed cancers in lung cancer screening - more than meets the eye
Devaraj A.
Eur Radiol. 2014 Sep 5. [Epub ahead of print] - “ The NLST randomized 53,454 older current or former heavy smokers to receive LDCT or chest radiography (CXR) for three annual screens. Participants were observed for a median of 6.5 years for outcomes. Vital status was available in more than 95% of participants. LDCT was positive in 24.2% of screens, compared with 6.9% of CXRs; more than 95% of all positive LDCT screens were not associated with lung cancer. LDCT detected more than twice the number of early-stage lung cancers and resulted in a stage shift from advanced to early-stage disease.”
Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial
Aberle DR, Abtin F, Brown K
J Clin Oncol. 2013 Mar 10;31(8):1002-8 - “Across 33 sites, the NLST enrolled 53,454 current or former smokers based on eligibility criteria of age 55 to 74 years and current or previous smoking history of a minimum of 30 pack-years (product of packs of cigarettes smoked daily and years of smoking). Former smokers had to have quit within the preceding 15 years.”
Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial
Aberle DR, Abtin F, Brown K
J Clin Oncol. 2013 Mar 10;31(8):1002-8 - “Participants were randomly assigned to receive either LDCT or CXR annually for three screens. Follow-up continued through December 31, 2009, for a median of 6.5 years. Diagnostic procedures, diagnoses, treatments, and outcomes were collected by manual abstraction of medical records on participants with positive screens and those with lung cancer diagnoses . Vital status was ascertained at least annually with confirmation by death certificates or query of the National Death Index.”
Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial
Aberle DR, Abtin F, Brown K
J Clin Oncol. 2013 Mar 10;31(8):1002-8 - “ The NLST randomized 53,454 older current or former heavy smokers to receive LDCT or chest radiography (CXR) for three annual screens. Participants were observed for a median of 6.5 years for outcomes. Vital status was available in more than 95% of participants. LDCT was positive in 24.2% of screens, compared with 6.9% of CXRs; more than 95% of all positive LDCT screens were not associated with lung cancer.”
Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial
Aberle DR, Abtin F, Brown K
J Clin Oncol. 2013 Mar 10;31(8):1002-8 - “Complications of LDCT screening were minimal. Lung cancer-specific mortality was reduced by 20% relative to CXR; all-cause mortality was reduced by 6.7%. The major harms of LDCT are radiation exposure, high false-positive rates, and the potential for overdiagnosis.”
Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial
Aberle DR, Abtin F, Brown K
J Clin Oncol. 2013 Mar 10;31(8):1002-8 - “This review discusses the risks and benefits of LDCT screening as well as an approach to LDCT implementation that incorporates systematic screening practice with smoking cessation programs and offers opportunities for better determination of appropriate risk cohorts for screening and for better diagnostic prediction of lung cancer in the setting of screen-detected nodules. The challenges of implementation are considered for screening programs, for primary care clinicians, and across socioeconomic strata.”
Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial
Aberle DR, Abtin F, Brown K
J Clin Oncol. 2013 Mar 10;31(8):1002-8 - NLST Trial Data
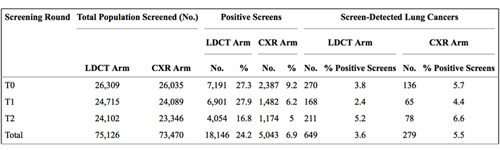
- “Overall, the NLST demonstrated the following: more lung cancers were detected with LDCT than with CXR; a stage shift was observed with LDCT, such that the absolute number of advanced-stage cancers was decreased relative to CXR; there was a 20% relative mortality reduction with LDCT compared with CXR, amounting to an absolute risk reduction of four individuals per 1,000 screened; there were few significant complications from LDCT screening; and a 6.7% reduction in all-cause mortality was observed with LDCT.”
Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial
Aberle DR, Abtin F, Brown K
J Clin Oncol. 2013 Mar 10;31(8):1002-8 - Challenges to Lung Cancer Screening
- Primary care providers will need to be convinced of the efficacy of lung cancer screening and that the benefits outweigh the risks the risks.
- Among the most challenging aspects of lung cancer screening implementation will be adoption by the community at risk.
- The diffusion of lung cancer screening across all socioeconomic strata will require a multipronged approach in which information strategies are used to educate across demographic divides. - “ Screening effectiveness is enhanced by identifying the optimal risk group most likely to harbor preclinical lung cancer. Between 80% and 90% of lung cancers occur in tobacco smokers, yet only 10% to 15% of chronic smokers develop lung cancer. Relative to smokers with normal lung function, those with chronic obstructive pulmonary disease (COPD) have up to a six-fold increased risk of lung cancer, making COPD by far the greatest known risk factor for lung cancer in ever-smokers.”.
Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial
Aberle DR, Abtin F, Brown K
J Clin Oncol. 2013 Mar 10;31(8):1002-8 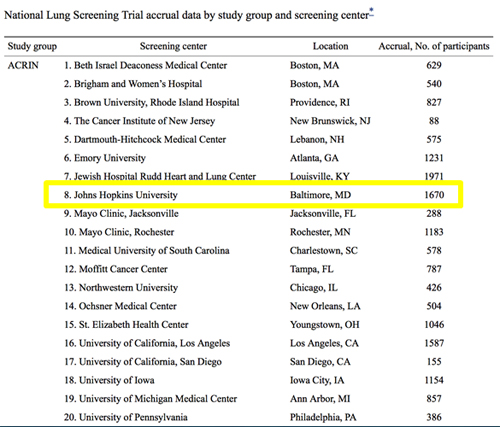
- Primary Result of NLST
- The NLST researchers found approximately 15 percent to 20 percent fewer lung cancer deaths among trial participants screened with low-dose helical CT relative to chest X-ray. This finding was highly significant from a statistical viewpoint, meaning it was due not to chance but rather to screening with helical CT. The 15 percent to 20 percent lower lung cancer death rate is equivalent to approximately three fewer deaths per 1,000 people screened in the CT group compared to the chest X-ray group over an average of 6.5 years of follow-up in the trial (17.6 per 1,000 versus 20.7 per 1,000). - Secondary Result of NLST
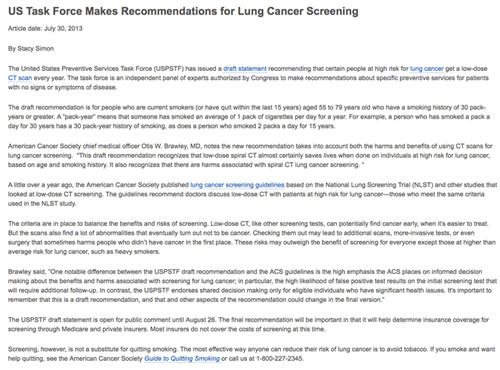
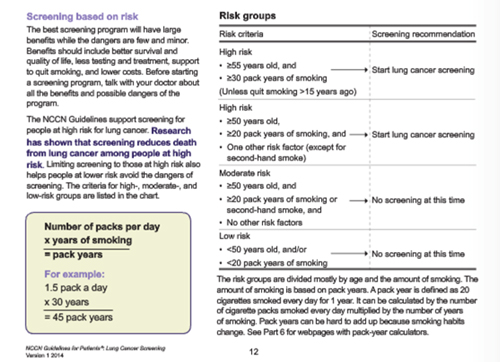
- An additional finding, which was not the main endpoint of the trial's design, showed that all-cause mortality (deaths due to any factor, including lung cancer) was 6.7 percent lower in those screened with low-dose helical CT relative to those screened with chest X-ray. This difference was largely due to the decrease in lung cancer mortality. - “The draft recommendation is for people who are current smokers (or have quit within the last 15 years) aged 55 to 79 years old who have a smoking history of 30 pack-years or greater. A “pack-year” means that someone has smoked an average of 1 pack of cigarettes per day for a year. For example, a person who has smoked a pack a day for 30 years has a 30 pack-year history of smoking, as does a person who smoked 2 packs a day for 15 years.”
- What about false positives?
- A positive screening result was defined as one in which a nodule or other finding was observed that was potentially related to lung cancer. On average, over all three screening rounds, 24.2 percent of the low-dose helical CTs were positive and 6.9 percent of the chest X-rays were positive and led to a diagnostic evaluation. Among people who had multiple annual screens (up to three screens) 39.1 percent had at least one positive screen in the CT arm and 16.0 percent had at least one positive screen in the chest X-ray arm. Diagnostic evaluation most frequently consisted of further imaging, and invasive procedures were rare. - What about false positives?
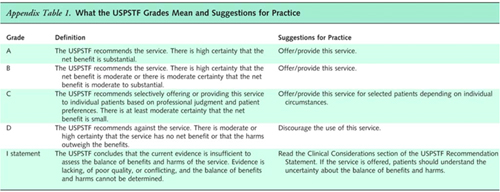
- Across the three rounds, when a positive screening result was obtained, 96.4 percent of the low-dose helical CT tests and 94.5 percent of the chest X-ray exams were false-positive, meaning that the observed finding was not due to lung cancer. These percentages varied little by round. The vast majority of false-positive results were probably due to the detection of benign lymph nodes or granulomata, which are non-cancerous inflamed tissue masses. The fact that these false-positive results were not cancer was usually confirmed noninvasively by the lack of change in the finding on follow-up CTs. - U.S. Preventive Services Task Force Recommendation Statement 12-31-2013
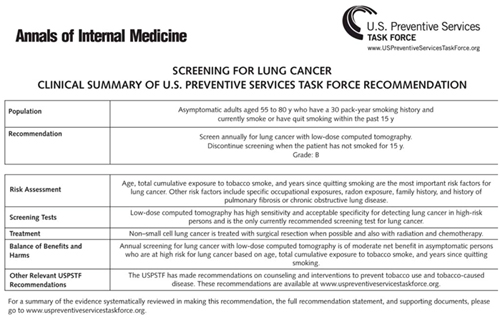
- The USPSTF recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults aged 55 to 80 years who have a 30 pack-year smoking history and currently smoke or have quit within the past 15 years. Screening should be discontinued once a person has not smoked for 15 years or develops a health problem that substantially limits life expectancy or the ability or willingness to have curative lung surgery. (B recommendation) - “ Results showed the majority of LDCT screening centers were located in the counties with the highest quartiles of lung cancer incidence and mortality in the Northeast and East North Central states, but several high-risk states had no or few identified screening centers including Oklahoma, Nevada, Mississippi, and Arkansas. As guidelines are implemented and reimbursement for LDCT screening follows, equitable access to LDCT screening centers will become increasingly important, particularly in regions with high rates of lung cancer incidence and smoking prevalence.”
Lung cancer screening using low-dose CT: The current national landscape.
Eberth JM1 et al.
Lung Cancer. 2014 Sep;85(3):379-84 - Low Dose CT Protocols
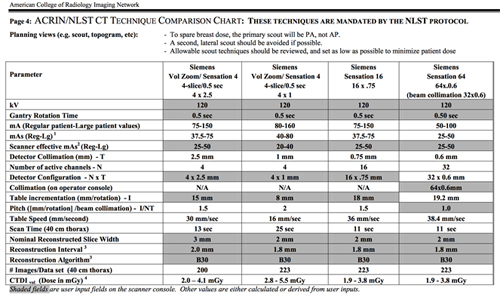
- NLST Time Capsule
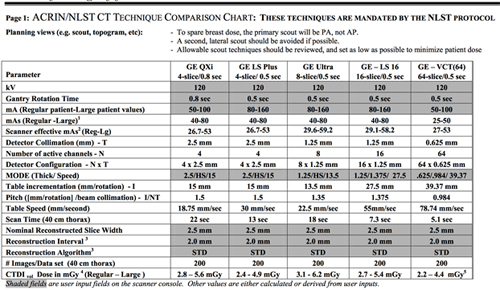
- NLST CT Interpretation
- Negative or minor abnormality: Not suspicious for lung cancer
- Clinically important abnormality: Not suspicious for lung cancer
- Positive: Suspicious for lung cancer - NLST Time Capsule
- CT Screening Scan Protocols 2014
- Our quantitative image analysis indicated that tube current, and thus radiation dose, could be reduced by 40% or 80% from ASIR or MBIR, respectively, compared with conventional FBP, while maintaining similar image noise magnitude and contrast-to-noise ratio.
- Radiation dose reduction for CT lung cancer screening using ASIR and MBIR: a phantom study
- Mathieu KB et al.
- J Applied Clin Med Physics, Vol 15, Number 2, 2014 
- NCCN Guidelines 2014
- Fleischner society pulmonary nodule recommendations
- Nodule size (mm) less than or equal to 4
- low risk patients - no follow-up needed
- high risk patients - follow-up at 12 months and if no change, no further imaging needed - Fleischner society pulmonary nodule recommendations
- Nodule size > 4-6 mm
- low risk patients - follow-up at 12 months and if no change, no further imaging needed
- high risk patients - initial follow-up CT at 6-12 months and then at 18-24 months if no change - Fleischner society pulmonary nodule recommendations
- Nodule size > 6-8 mm
- low risk patients - initial follow-up CT at 6-12 months and then at 18-24 months if no change
- high risk patients - initial follow-up CT at 3-6 months and then at 9-12 and 24 months if no change - Fleischner society pulmonary nodule recommendations
- Nodule size > 8 mm
- either low or high risk patients
- follow-up CTs at around 3, 9, and 24 months
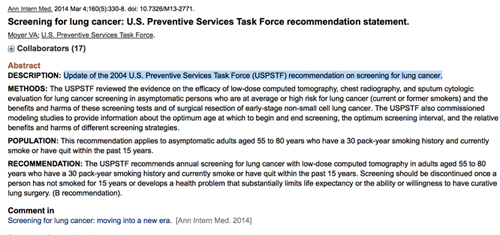
- dynamic contrast enhanced CT, PET, and/or biopsy - “The USPSTF recommends annual screening for lung cancer with low-dose computed tomography in adults aged 55 to 80 years who have a 30 pack-year smoking history and currently smoke or have quit within the past 15 years. Screening should be discontinued once a person has not smoked for 15 years or develops a health problem that substantially limits life expectancy or the ability or willingness to have curative lung surgery. (B recommendation).”
Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement.
Moyer VA et al.
Ann Intern Med. 2014 Mar 4;160(5):330-8 - “This recommendation applies to asymptomatic adults aged 55 to 80 years who have a 30 pack-year smoking history and currently smoke or have quit within the past 15 years.”
Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement.
Moyer VA et al. - Ann Intern Med. 2014 Mar 4;160(5):330-8
- May 2014 Lung Cancer Screening and Medicare
- Lung Cancer is the number 1 cause of cancer related deaths
- In 2011 (the most recent year numbers are available from the CDC)
- 207,339 people in the United States were diagnosed with lung cancer, including 110,322 men and 97,017 women.
- 156,953 people in the United States died from lung cancer, including 86,736 men and 70,217 women. - Lung Cancer and Smoking
(NCI database)
- Cigarette smoking causes an estimated 443,000 deaths each year, including approximately 49,000 deaths due to exposure to secondhand smoke.
- Lung cancer is the leading cause of cancer death among both men and women in the United States, and 90 percent of lung cancer deaths among men and approximately 80 percent of lung cancer deaths among women are due to smoking. - Lung Cancer and Smoking
(NCI database)
- Smoking causes many other types of cancer, including cancers of the throat, mouth, nasal cavity, esophagus, stomach, pancreas, kidney, bladder, and cervix, and acute myeloid leukemia.
- People who smoke are up to six times more likely to suffer a heart attack than nonsmokers, and the risk increases with the number of cigarettes smoked. Smoking also causes most cases of chronic lung disease.
- People who quit smoking, regardless of their age, are less likely than those who continue to smoke to die from smoking-related illness:
- Quitting at age 30: Studies have shown that smokers who quit at about age 30 reduce their chance of dying prematurely from smoking-related diseases by more than 90 percent
- Quitting at age 50: People who quit at about age 50 reduce their risk of dying prematurely by 50 percent compared with those who continue to smoke
- Quitting at age 60: Even people who quit at about age 60 or older live longer than those who continue to smoke
Colon
- Diverticular Disease: Facts
- Incidence of diverticulosis increases substantially with age
- Most common cause of hematochezia in the elderly
- Diverticular bleeding is usually arterial, and can be massive and severe
- Even if active bleeding is not visualized, the presence of many colonic diverticula should be suggestive of cause of bleeding
- Ischemic Colitis: Facts
- Compromise of mesenteric blood supply leading to colonic injury
- Elderly, cardiac patients
- More commonly hypoperfusion (not embolic)
- Diagnostic clue:
- Pneumatosis
- Mesenteric venous gas
- Symmetric bowel wall thickening
- Thumbprinting on CT - Misty Mesentery:Facts
- Pancreatitis
- Fibrosing (retractile) mesenteritis
- GI tract (appendicitis, diverticulitis, etc.)
- Peritonitis (bacterial, TB, etc.)
- Toxic Megacolon: Facts
- Acute transmural fulminant colitis with neuromuscular degeneration and colonic dilatation
- Dilated ahaustral colon with pseudopolyps and air-fluid levels
- No specific diameter although often markedly dilated
- Patients are sick - Ulcerative Colitis: Federle Facts
- Chronic, idiopathic diffuse inflammatory disease
- Primarily involves colorectal mucosa and submucosa
- Diagnostic clue: pancolitis with decreased haustration and multiple ulcerations
- Location:
- Rectum (30%)
- Rectum + colon (40%)
- Pancolitis (30%) - Large Bowel Infections: Facts
- Number of different possible etiologies including pseudomembranous colitis, bacterial organisms (campylobacter, shigella, salmonella, E. coli, etc.) and parasites (E. histolytica)
- Clostridium difficile is by far the most common in daily practice
- Often arises in the setting of prior antibiotic therapy or chemotherapy
- Can be a fulminant colitis with high morbidity and mortality, and not uncommonly presents with GI bleeding
- Pancolitis with extensive pericolonic fat stranding, free fluid, and inflammatory change.
- Isolated involvement of right or transverse in up to 5% of cases - Aorto-Enteric Fistulae: Facts
- Life-threatening disorder with mortality of virtually 100%
- Primary or secondary forms
- Secondary most common – prior aortic surgery or raft placement
- Classic triad: Abdominal pain, massive GI hemorrhage, and pulsatile abdominal mass
- CT is the best initial modality:
- Ectopic gas within aortic lumen or adjacent to aorta
- Direct contrast extravasation from aorta to bowel or vice-versa is rare
- Effacement of fat plane between the aorta and adjacent bowel
- Focal bowel wall thickening adjacent to the aorta
- Periaortic soft tissue thickening and fluid, - Stercoral Colitis: Facts
- Primarily seen in elderly patients
- Overdistension of rectal lumen from impacted stool
- Increased luminal pressure results in rectal wall ischemia (disrupts blood supply)
- Ulcers of rectal wall result in bleeding and perforation
- Affects up to 6% of elderly patients in long-term care
- Active extravasation almost never visualized
- Slow, intermittent bleeding
- MDCT shows distended rectum with wall thickening and perirectal stranding
Kidney
- “RAAs are extremely rare clinical entities, which constitute localized dilations of renal arteries and/or branches. RAAs can be classified into 4 basic categories: the saccular, fusiform, dissecting, or intrarenal,and saccular RAA is the most common type.”
Rupture of Renal Artery Aneurysm: A Rare Urologic Emergency Entity
Zhou H et al.
DOI: 10.1016/j.urology.2014.08.002 - “ Predisposing factors encompass congenital malformations of the kidneys, untreated hypertension, atherosclerosis, pregnancy, trauma, malignancy, renal angiomyolipoma, radiation, and consumption of cyclophosphamide.”
Rupture of Renal Artery Aneurysm: A Rare Urologic Emergency Entity
Zhou H et al.
DOI: 10.1016/j.urology.2014.08.002 - “There is an increased mortality in type IV EDS, mostly because of vascular complications such as spontaneous arterial rupture, aneurysmal degeneration with subsequent rupture or dissection, and arteriovenous fistulas.”
Thromboembolic renal infarction due to a renal artery aneurysm in a patient with Ehlers-Danlos syndrome type IV
Abramowitz Y et al.
Eur J Vascular Med Vol 17, Issue 5, August 2006, Pages 377–379
Liver
- Biliary Cystadenoma/Cystadenocarcinoma
- Cystic lesion with multiple internal loculations
- Encapsulated and well circumscribed
- Even if benign, can have malignant potential
- Very difficult to completely resect
- Female predominance
- Cholangiocarcinoma
- Tumor arises from the bile duct epithelium
- 95% adenocarcinoma
- Associated with:
- PSC
- Choledochal cysts
- Drug exposures (such as thoratrast)
- Congenital hepatic fibrosis
- Viral hepatitis - Cholangiocarcinoma
- Intrahepatic
- Mass forming intrahepatic cholangiocarcinoma
- Periductal infiltrating cholangiocarcinoma
- Intraductal cholangiocarcinoma
- Hilar Cholangiocarcinoma
- Extrahepatic Cholangiocarcinoma - Cholangiocarcinoma
- Variable appearance
- Peripheral hypervascularity on arterial phase images (and sometimes venous phase)
- Hypovascular lesions
- Delayed enhancement
- Dilated bile ducts (with bile duct thickening)
- Capsular retraction
- Lobar or segmental atrophy
- Metastases
- Hypervascular metastases: “MR CT PET”
- M – Melanoma
- R – Renal cell carcinoma
- C – Choriocarcinoma
- T – Thyroid cancer
- PET – Neuroendocrine tumor
- Use MIP images to identify subtle lesions
- Approach to small hepatic hypodensities
- Jones et al looked at 1454 outpatients with a contrast-enhanced CT
- 17% had a TSTC (< 15 mm)
- In patients without a known malignancy, 100% were benign
- Schwartz et al looked at CT scans for 2978 patients with cancer
- 12.7% had a TSTC
- 80% were benign
- 12% were malignant
- TSTC’s metastatic in 22% of breast cancer patients
- Hepatic Adenoma
- Female predominance
- Highly associated with OCP use, steroids, steatosis, and glycogen storage disease
- Can present with hemorrhage in 20%
- Primarily composed of hepatocytes and Kuppfer cells
- Hepatic “adenomatosis” without OCP use
- Malignant degeneration to HCC rare - Hepatic Adenoma
- Hepatic artery vascular supply
- Heterogeneously hypervascular on the arterial phase
- Fat
- Hemorrhage
- Variable appearance on venous and delayed images
- Often encapsulated on venous and delayed images
- Can have a central scar - FNH versus Adenoma
FNH
-Common lesion
-Homogeneously enhancing
-No fat
-No hemorrhage
-No capsule
-No calcification
Adenoma
-Rare lesion
-Heterogeneous (when large)
-Fat
-Hemorrhage
-Capsule
-Can calcify (prior hemorrhage)
- Hepatocellular Carcinoma: Facts
- 3rd leading cause of death worldwide
- Strong male predilection
- Risk factors:
- Hepatitis B and C
- Cirrhosis
- Fatty liver
- Management options
- Surgery, chemoembolization, transplant - HCC – Criteria for Liver Transplant
Milan Criteria
- Single lesion ? 5 cm
- 3 lesions smaller than 3 cm
- No vascular invasion
- No metastatic disease outside of the liver
UCSF Criteria
- Single lesion ? 6.5 cm
- 3 lesions smaller than 4.5 cm
- No vascular invasion
- No metastatic disease outside of the liver - Fibrolamellar HCC
- Young patients without cirrhosis
- Theoretically less aggressive
- Large, aggressive looking (lobulated)
- Hypervascular with delayed washout
- Encapsulated
- Central scar – Ca++
- Adenopathy common
- “The right indications for surgery remain rupture, intratumoral bleeding, Kasabach-Merritt syndrome and organ or vessels compression (gastric outlet obstruction, Budd-Chiari syndrome, etc.) represents the valid indication for surgery and at the same time they are all complications of the tumor itself. The size of the tumor do not represent a valid indication for treatment.”
What is changing in indications and treatment of hepatic hemangiomas. A review.
Toro A et al.
Ann Hepatol. 2014 Jul-Aug;13(4):327-39. - “ Liver hemangiomas, when indication exist, have to be treated firstly by surgery (hepatic resection or enucleation, open, laproscopic or robotic), but in the recent years other therapies like liver transplantation, radiofrequency ablation, radiotherapy, trans-arterial embolization, and chemotherapy have been applied.”
What is changing in indications and treatment of hepatic hemangiomas. A review.
Toro A et al.
Ann Hepatol. 2014 Jul-Aug;13(4):327-39. - “ In conclusion, at two-phase spiral CT, the most common contrast-enhancement patterns of hemangioma are peripherally nodular high and/or uniform high during the arterial and portal venous phases. However, hemangiomas smaller than 2 cm may have atypical enhancing patterns including low and iso-attenuation.”
Hepatic hemangioma: contrast-enhancement pattern during the arterial and portal venous phases of spiral CT.
Yun EJ et al.
Abdom Imaging. 1999 May-Jun;24(3):262-6. - “The incidence of hemangiomas is 2–7% in the general population. Hemangiomas are the most frequent benign hepatic tumors and are usually found in patients aged between 40 and 60 years, more frequently in women. In 30–35% of patients the lesions are multiple. If larger than 4–10 cm, they are termed ‘giant’ hemangiomas.”
Giant hemangiomas of the liver: surgical strategies and technical aspects
Berloco P et al.
HPB (Oxford). 2006; 8(3): 200–201.
Radiation Dose
- Iterative Reconstruction
- Iterative reconstruction techniques have recently been introduced which reduce image noise
- This noise reduction allows studies to be acquired at significantly lower dose, but with image quality comparable to FBP images acquired at higher doses
- Thin-section images, which are normally difficult to interpret when reconstructed with FBP (as a result of image noise), are less noisy and of better diagnostic quality when reconstructed with iterative reconstruction. - Iterative Reconstruction
- “Correction” loops are extremely time-consuming
- Particularly true with early algorithms, which performed reconstructions only in “raw data space”
- Algorithms now much faster as a result of performing reconstructions in both “raw data space” and “image space”
- Markedly speeds up reconstruction time and makes IR clinically viable
- Some manufacturers “blend” FBP with IR to reduce reconstruction times and to make images look more like traditional FBP images - Patient Positioning
- Improper centering of patients (either vertically or laterally) can increase surface dose by 23% and noise by 7%.
- Even a small amount of miscentering can have dramatic effects on dose
- Particularly a problem if AEC is used, as doses will be increased to compensate for noise. - Patient Positioning
- Must be especially careful with small and pediatric patients.
- Effect of miscentering increases if you are using your scanner in dual-source mode.
- Scoliotic patients and unconscious ICU patients also problematic
Patient Positioning
- Bowtie filters normally compensate for patient attenuation during tube rotation
- increased x-ray intensity to the thickest parts of the patent (i.e. center of the patient)
- decreased intensity to the thinnest parts of a patient (i.e. the patient surface).
- Bowtie filter functions under the assumption that the patient is correctly centered within the gantry
- When patient is improperly positioned, the mathematical assumptions underlying this filter break down, and doses to the surface of the body increase.
- CTDIvol
- Measures the radiation output or energy delivered by the scanner to tissue
- Not truly radiation dose
- CTDIvol is measured on plastic cylinder phantoms (16 or 32 cm)
- CTDIvol measurements are made by the manufacturer on phantoms
- Calculated at scanner based on the scan parameters being used - CTDIvol
- Allows comparison of different protocols with different scan parameters
- Described in units of Gray (Gy) or milligray (mGy) – energy per kg of mass
- Would only be a reasonable estimate of dose if patient were composed of plastic and was same size as phantom
- Does not take into account scan length
- Does not take into account patient size, attenuation, or shape - Dose-Length Product (DLP)
- Better accounts for overall energy delivered by any given protocol
- DLP(mGy.cm) = CTDIvol x scan length (cm)
- Hence, unlike CTDIvol, DLP takes into account scan length
- CTDIvol might be same for CT Abd and CT Abd/Pelvis, but DLP would be higher in the latter exam - Dose-Length Product (DLP)
- Changing CT scan parameters will change both CTDIvol and dose-Length Product (DLP).
- Changing scan length will only change DLP
- DLP is a better measure of the radiation risk of an examination
- Allows you to calculate effective dose - Effective Dose (E)
- Biologic effects of radiation depend not only on radiation imparted, but also on biologic sensitivity of an organ
- Unlike DLP and CTDIvol, better answers question: “What are the chances the patient wil be harmed by scan?”
- Allows comparison with other radiation risk (i.e. background)
- Units of effective dose is Sievert (Sv) or millisievert (mSv) - Effective Dose (E)
- E = DLP x k (weighting factor)
- Annual background radiation is roughly 3 mSv
- Natural radiation in rocks, soil, radon gas, space, etc. - Tube Current (mAs) and Automatic Tube Current Modulation (AEC)
- Increases in product of tube current and scan time (mAs) improve image quality and reduce noise
- Linear relationship between tube current and dose
- Can be manually controlled, but AEC is now available on virtually all scanners.
- Increases mAs in parts of the body with higher attenuation (i.e. shoulder & hips)
- Decreases mAs in parts of body with lower attenuation (i.e. abdomen & thorax). - Automatic Exposure Control (AEC)
- Patient size modulation varies the mAs based on a global evaluation of the overall size of the patient as seen on the scout radiograph.
- Z-axis modulation changes the mAs constantly along the Z-axis of the patient depending on the patient attenuation at each point, as determined using the scout image.
- Angular (x, y) modulation changes the mAs as the x-ray tube rotates 360 degrees around the patient to account for different attenuations in different projections of the x-ray beam.
- Combined x-y-z modulation adjusts the mAs in all three axes based on the patient’s attenuation. - Automatic Exposure Control (AEC)
- Be careful with small or pediatric patients
- Improper centering can result in increased image noise and low mAs
- Check to see if your vendor’s software can take into account metallic hardware
- Acceptable noise levels should be varied depending on the type of scan
- Be careful with obese patients
- “Cap” the tube current or else mAs may be increased markedly with increased dose - Tube Potential (kVp)
- Radiation dose changes with the square of the tube potential
- Reducing kVp from 120 to 100 reduces dose by 33%
- Reducing kVp from 120 to 80 reduces dose by 65%
- Reductions in kVp can increase attenuation of iodine
- Approach k-edge of iodine and photoelectric effect
- Can potentially improve contrast-to-noise ratios in some cases - Tube Potential (kVp)
- No predictable relationship between kVp and image noise
- Can result in non-linear exponential increases in image noise
- Will require increases in mAs in most cases to preserve diagnostic quality
- Must adjust reference mAs or noise index to increase tube current - Tube Potential
- Low kVp protocols most useful in thin-non-obese patients
- Very useful in vascular or angiographic studies
- Improved conspicuity of iodine
- Requires some trial-and-error, as there is no formula to determine when to reduce kVp
- SCCT recommends kVp of 100 in cardiac CT for patients weighing under 90 kg - Reconstruction Algorithm
- “Filtered back projection” (FBP) is the traditional method of CT reconstruction
- Used to reconstruct “Projection data” (i.e. raw data from the scanner) into a final image
- Assumes a perfect relationship between raw data and final image
- This assumption only holds true with high radiation doses and low image noise - Pitch
- Pitch = Table travel per rotation
- Pitch < 1 : Overlap between acquisitions
- Pitch > 1 : Gaps between acquisitions
- Pitch =1 : Acquisitions are contiguous
- Smaller pitch, with increased overlaps and sampling at each location, increases radiation dose
- Improved signal-to-noise and contrast-to-noise
- Larger pitch decreases dose in a linear fashion. - Pitch
- For most body applications, a pitch of roughly 1 is acceptable
- Higher pitches (i.e. > 1.5) result in interpolation artifacts and increased image noise
- Lower pitches (~ 0.5) in cardiac applications
- Overcomes motion artifacts and necessitated by reconstruction algorithms - High Pitch Mode
- Higher pitches (i.e. FLASH mode) now available on latest scanners (dual-source)
- Pitches up to 3.4 now available
- Fast scan times and decreased motion artifacts
- Significant dose reductions compared to retrospective or prospective gating for vascular studies
- Apfalterer et al found dose reduction of 45-50% for vascular studies
Vascular
- “RAAs are extremely rare clinical entities, which constitute localized dilations of renal arteries and/or branches. RAAs can be classified into 4 basic categories: the saccular, fusiform, dissecting, or intrarenal,and saccular RAA is the most common type.”
Rupture of Renal Artery Aneurysm: A Rare Urologic Emergency Entity
Zhou H et al.
DOI: 10.1016/j.urology.2014.08.002 - “ Predisposing factors encompass congenital malformations of the kidneys, untreated hypertension, atherosclerosis, pregnancy, trauma, malignancy, renal angiomyolipoma, radiation, and consumption of cyclophosphamide.”
Rupture of Renal Artery Aneurysm: A Rare Urologic Emergency Entity
Zhou H et al.
DOI: 10.1016/j.urology.2014.08.002 - “There is an increased mortality in type IV EDS, mostly because of vascular complications such as spontaneous arterial rupture, aneurysmal degeneration with subsequent rupture or dissection, and arteriovenous fistulas.”
Thromboembolic renal infarction due to a renal artery aneurysm in a patient with Ehlers-Danlos syndrome type IV
Abramowitz Y et al.
Eur J Vascular Med Vol 17, Issue 5, August 2006, Pages 377–379
