High value MDCT angiography of acute superior mesenteric artery pathology: What the emergency medicine physician and vascular interventionist need to knowHigh value MDCT angiography of acute superior mesenteric artery pathology: What the emergency medicine physician and vascular interventionist need to know Elliot K. Fishman, MD, FACR The Russell H. Morgan Department of Radiology and Radiological Science The Johns Hopkins Medical Institutions Baltimore, Maryland |
Imaging technique: Role of multi-planar reconstructions
 |
Acute Mesenteric Ischemia (AMI)
|
Acute Mesenteric Ischemia (AMI) Illustration demonstrating thrombosis of the SMA with sharp vessel cut-off.  |
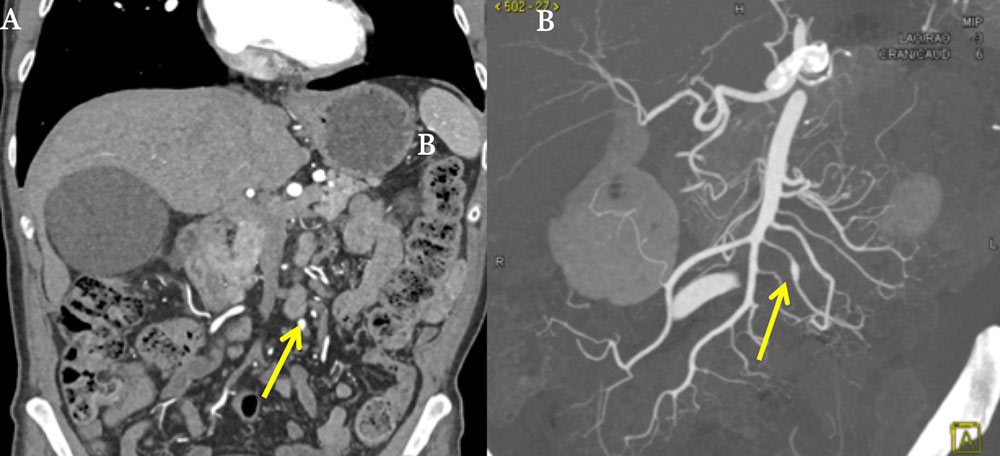
Acute Mesenteric Ischemia (AMI): MPRs 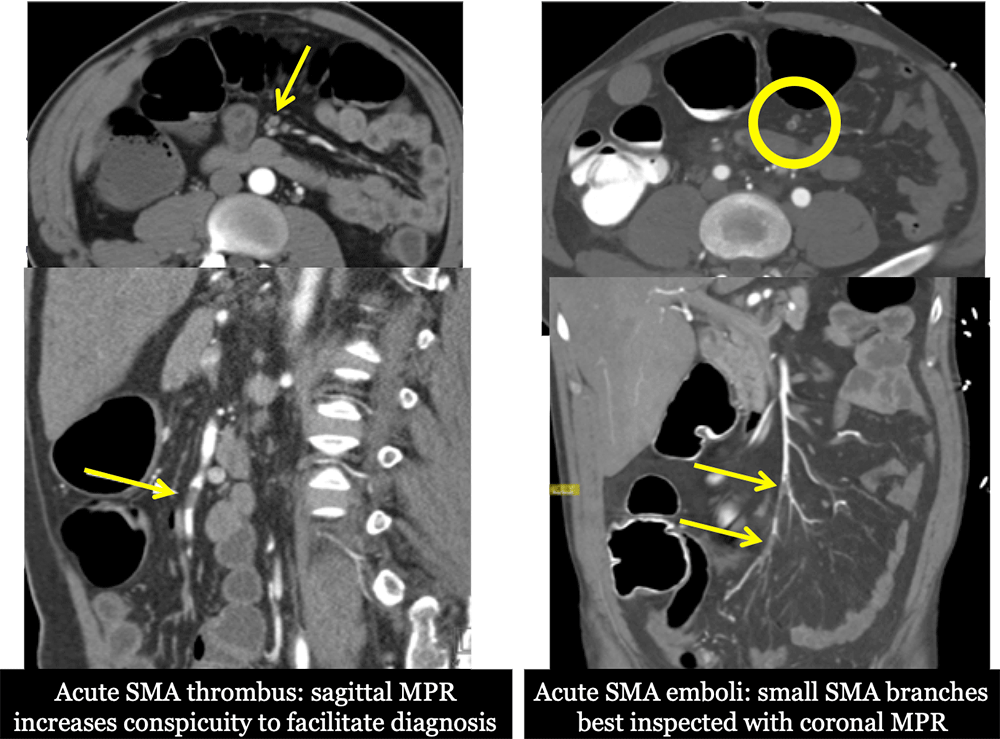 |
Acute Mesenteric Thrombosis 82-year-old male with a history of HTN, sick sinus syndrome and idiopathic cardiomyopathy who presented with severe abdominal pain, diarrhea, and emesis, elevated lactate level and acute kidney injury. Coronal (A), sagittal (B), and MIP (C) CT images demonstrate thrombosis and complete occlusion of the distal SMA with a sharp cutoff (red arrow). 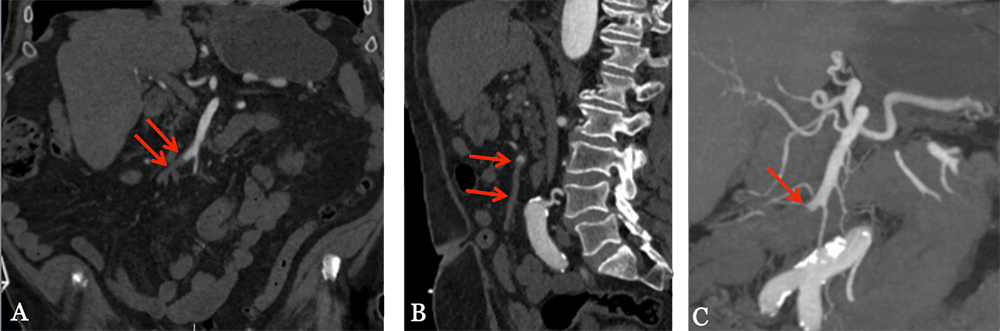 |
Chronic Mesenteric Ischemia (CMI)
 Illustration demonstrating atherosclerotic plaque narrowing the proximal 2 cm of SMA near the ostium |
Chronic SMA Thrombosis 56-year-old male with a history of HTN, HLD, CAD, and COPD who presents with severe postprandial abdominal pain. He has started to avoid meals and lost 10 pounds in the past month. Coronal (A), sagittal (B), MIP (C), and volume rendering (D) CT images demonstrate an approximately 2 cm segment of occlusive thrombus within the proximal SMA. The SMA reconstitutes distally by several collateral vessels. 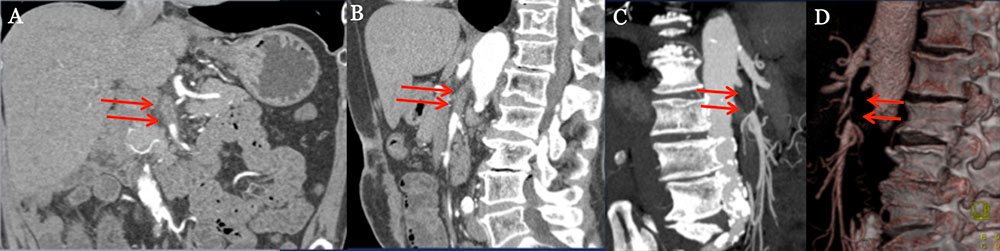 |
SMA Dissection
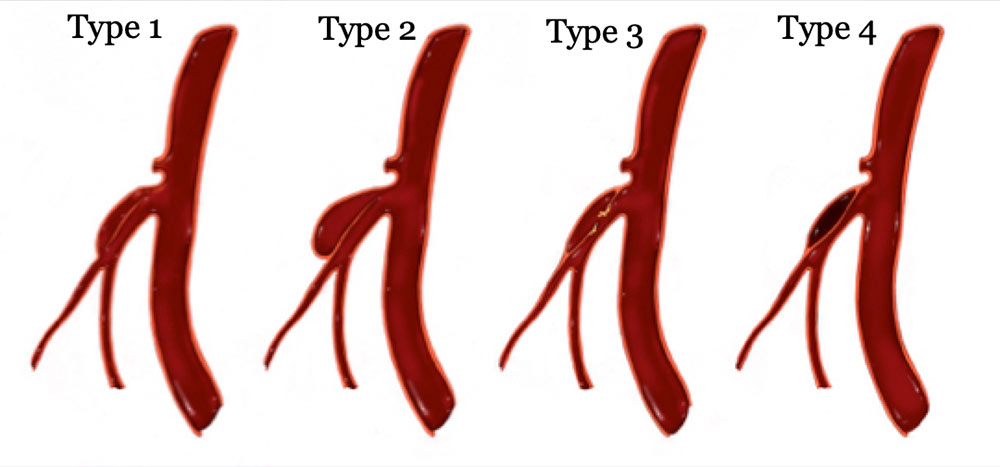 |
SMA Dissection 48-year-old female who presents with diffuse abdominal pain and tearing back pain associated with nausea and vomiting. Axial (A) and sagittal (B) CT images demonstrate a short segment nonocclusive type II dissection of the mid SMA (red arrows) without bowel wall thickening or ischemia, amenable to stenting. The 3D volume rendering sagittal (C) and coronal (D) CT images depict the extent of the dissection (yellow arrows). 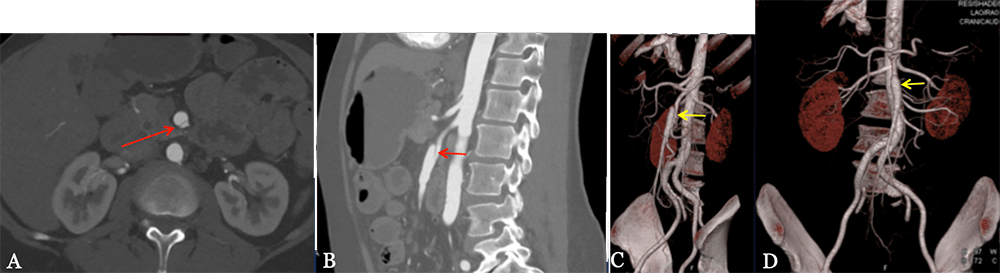 |
SMA Dissection 56-year-old male with Marfan syndrome. Sagittal images (A and B) demonstrating the long segment of SMA dissection with the flap extending 11 cm. An aneurysm of the mid-SMA measuring 1.7 cm is identified by the yellow arrows. The false lumen is patent and provides flow to multiple intestinal branches. The start of the dissection flap (blue arrow) is 1.4 cm from the origin of the SMA. All findings are important to know for possible endovascular treatment. 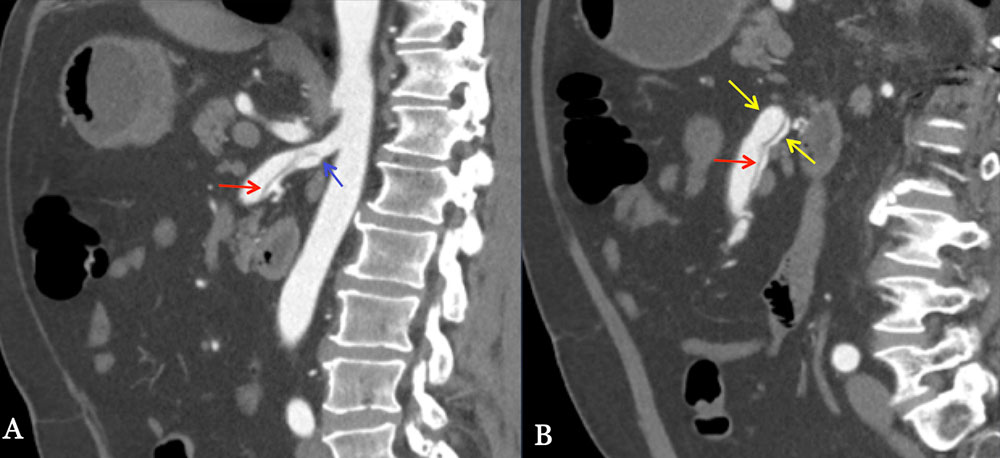 |
SMA Dissection 49-year-old male who presents with acute onset abdominal pain radiating to his back pain. Coronal (A and B) and sagittal (C) CT images demonstrate a proximal dissection of the SMA (red arrow) extending into jejunal and ileal branches (yellow arrows). Thrombosed and dilated proximal false lumen depicted by the blue arrow. Near complete occlusion of the distal SMA (orange arrow). 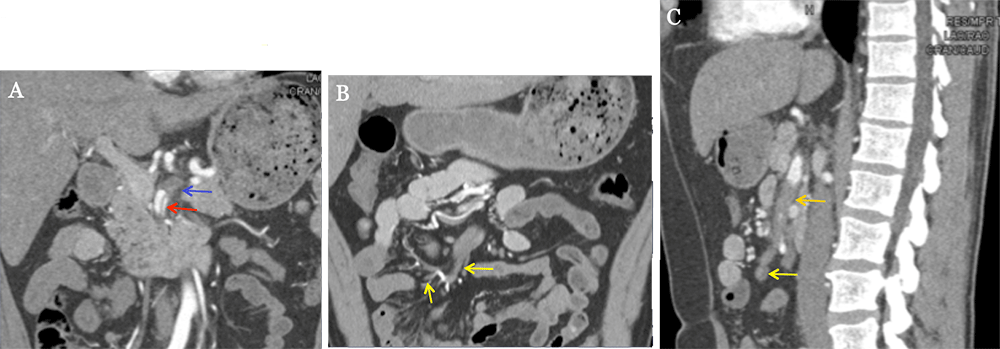 |
SMA Dissection 59-year-old male with a type B aortic dissection. Axial image (A) and the volume rendering 3D image demonstrate the descending aorta dissection flap (red arrow) involving the SMA (yellow arrow), precluding primary repair with endovascular stenting. The volume rendering 3D image depicts the blind ending false lumen with intestinal branches (blue arrow). 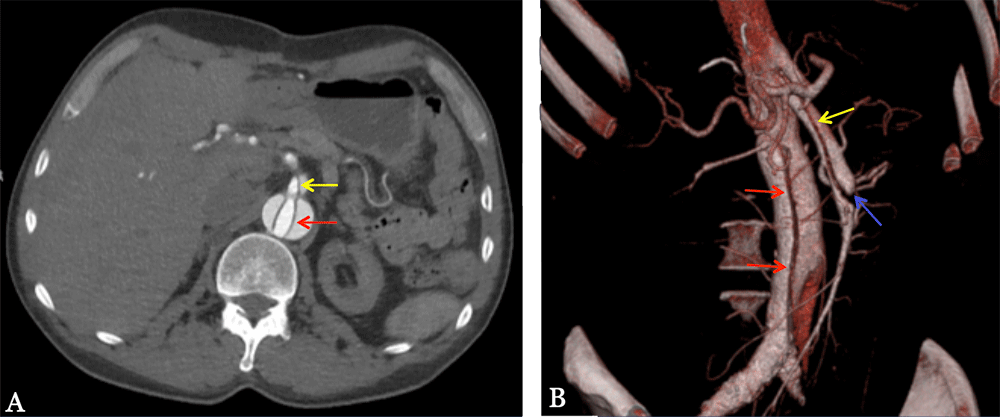 |
SMA Aneurysm 29-year-old male with a history of Loeys-Dietz syndrome who presents with abdominal pain, nausea, and vomiting. Axial (A), sagittal (B), and 3D rendering (C) CT images demonstrate fusiform aneursymal dilation of the proximal SMA measuring up to 3.5 cm (red arrows) with dilation of the more distal SMA to 1.2 cm (yellow arrows). Minimal wall thickening and fat stranding surrounding the proximal SMA. Tortuosity and dilation of the abdominal aorta and common iliac arteries. 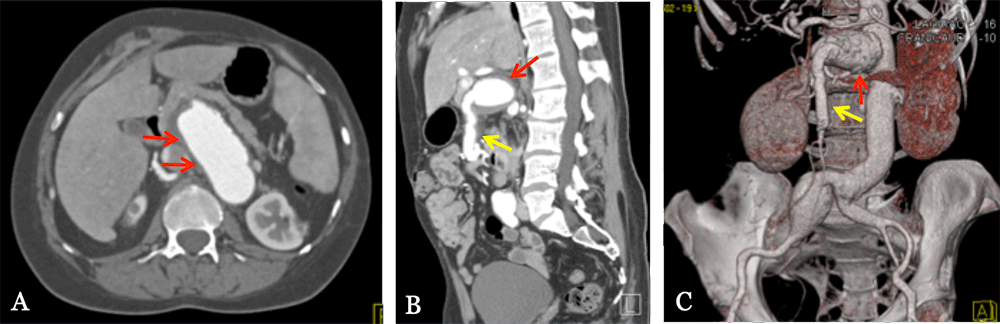 |
SMA Aneurysm 82-year-old male with proximal celiac artery occlusion who presents with peri-umbilical abdominal pain. Axial (A) image demonstrates a calcified enhancing lesion arising from an unclear vessel (red arrow). Multiple collateral vessels arising from the pancreaticoduodenal arcade. The sagittal MIP (B) image more clearly demonstrates a saccular aneurysm of a proximal SMA branch measuring up to 1.7 cm (red arrows). 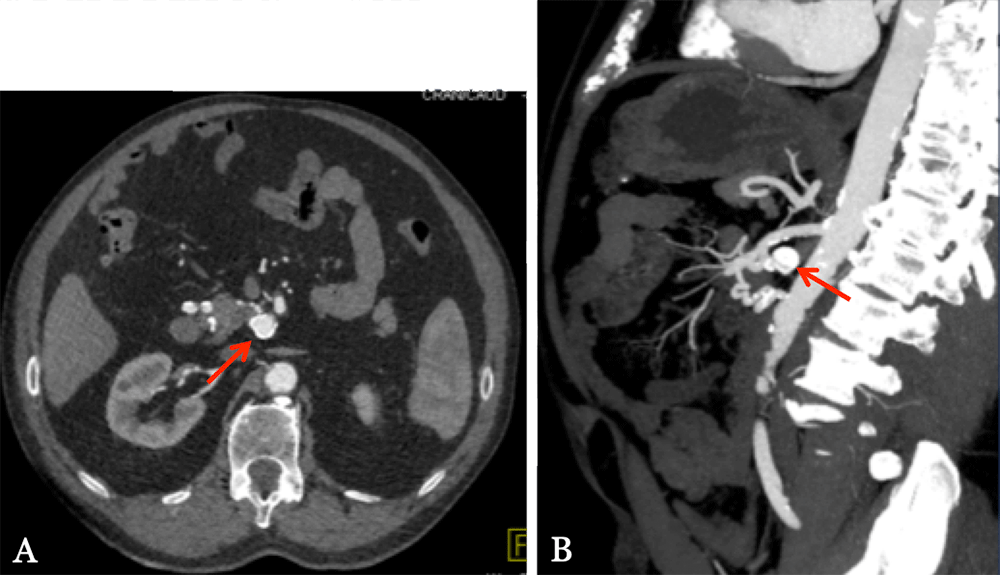 |
SMA Aneurysm 69-year-old male with abdominal pain and an incidental aneurysm found at outside hospital. Sagittal image (A) demonstrates a partially thrombosed aneurysm of the SMA (red arrow). The sagittal MIP image (B) easily depicts the aneurysm is 4.2 cm from the SMA origin. Volume rendering 3D image (C) shows the location of the aneurysm in relation to the branches of the SMA and the pancreas. 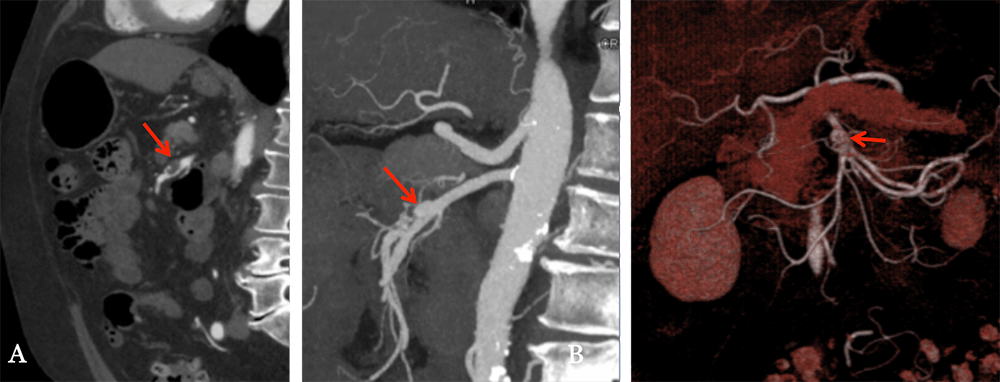 |
SMA Vasculitis 70-year-old female with a history of Takayasu’s arteritis who presents with abdominal pain. Sagittal MPR shows proximal circumferential narrowing (arrow). Endovascular treatment may be attempted if medical management fails. 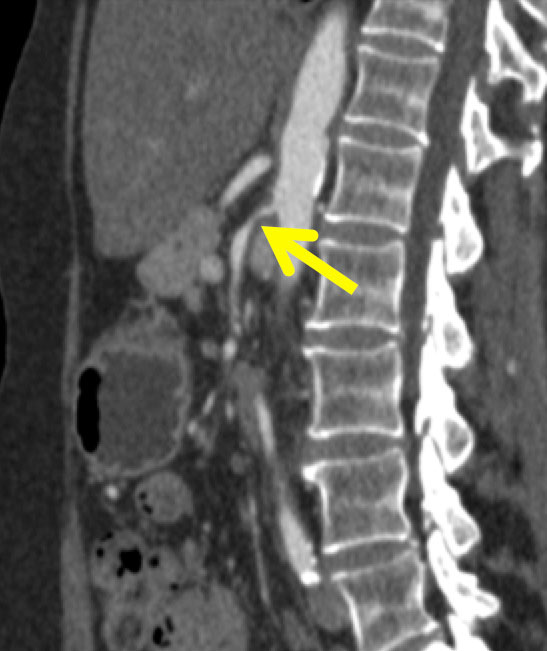 77-year-old female with a history of giant cell arteritis who presents with weight loss. Sagittal MIP image shows the long segment circumferential narrowing (arrow) without critical stenosis. Endovascular treatment is not advised for this patient. 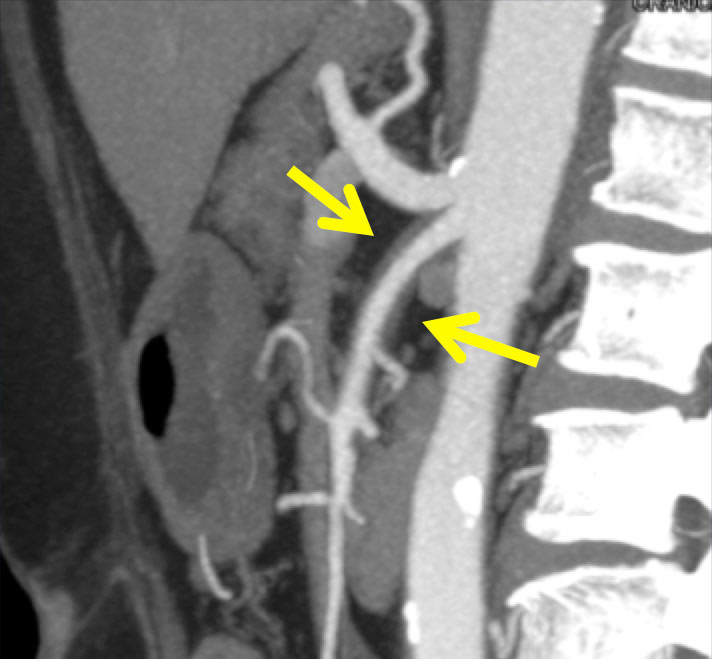 |
SMA Vascular Territory Illustration demonstrating SMA vascular territory from near the ligament of treitz to the proximal two-thirds of the transverse colon. 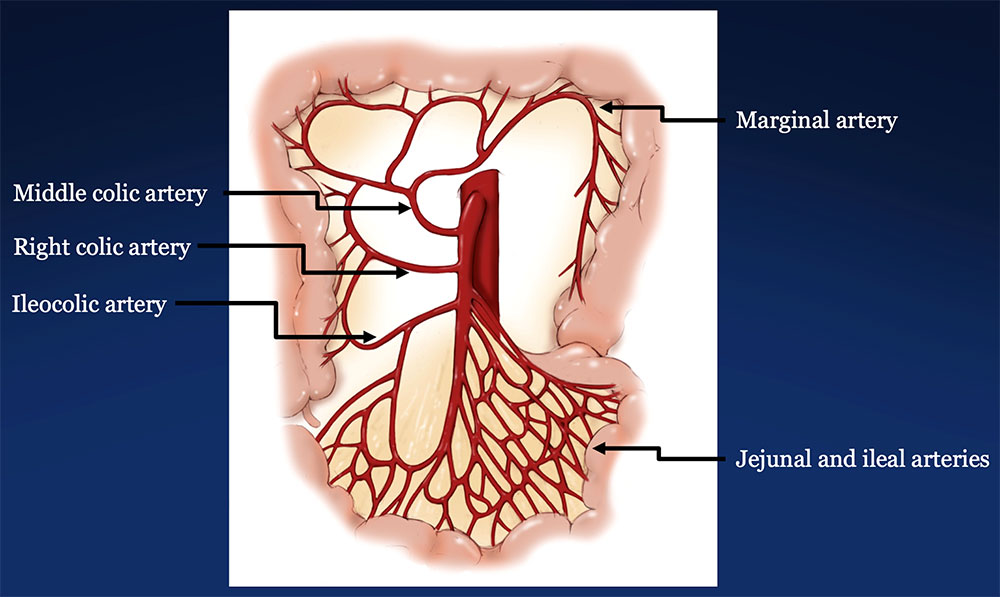 |
SMA Hemorrhage 76-year-old male with a history of rectal adenocarcinoma status post low anterior resection and recent diverting ileostomy takedown who presents with large volume bright red blood per rectum. Axial (A and D), coronal (B and E), and sagittal (C and F) CT images in the arterial (A-C) and venous (D-F) phase demonstrate contrast extravasation at the site of ileal anastomosis in the RLQ with pooling of blood. 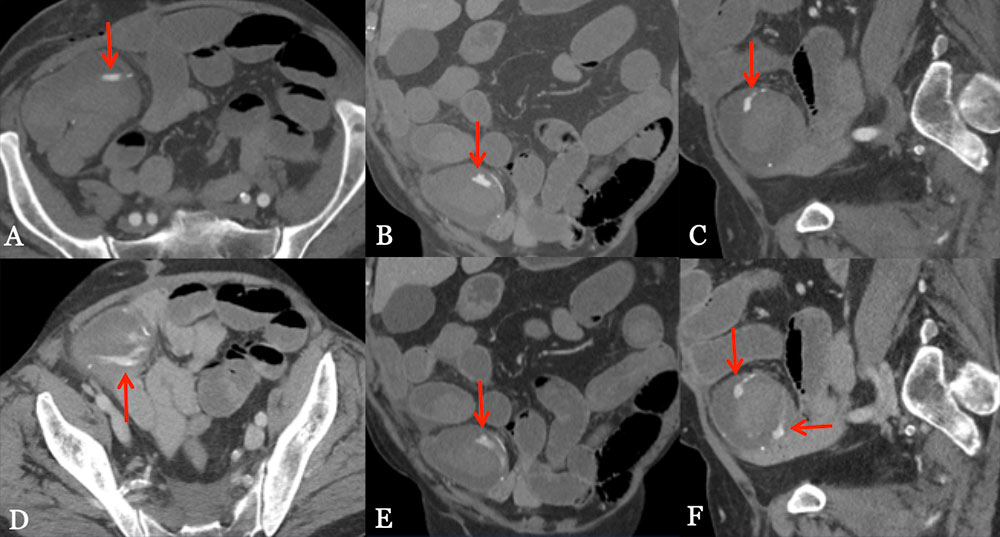 |
SMA Hemorrhage 84-year-old male with a history of atrial fibrillation and sick sinus syndrome who presents with bright red blood per rectum. Axial (A and C) and coronal (B and D) CT images in the arterial (upper images) and venous (lower images) phase demonstrate hyperdense material in the ascending colon as well as within a diverticulum that increases on venous phase, compatible with a bleeding diverticulum (red arrows). 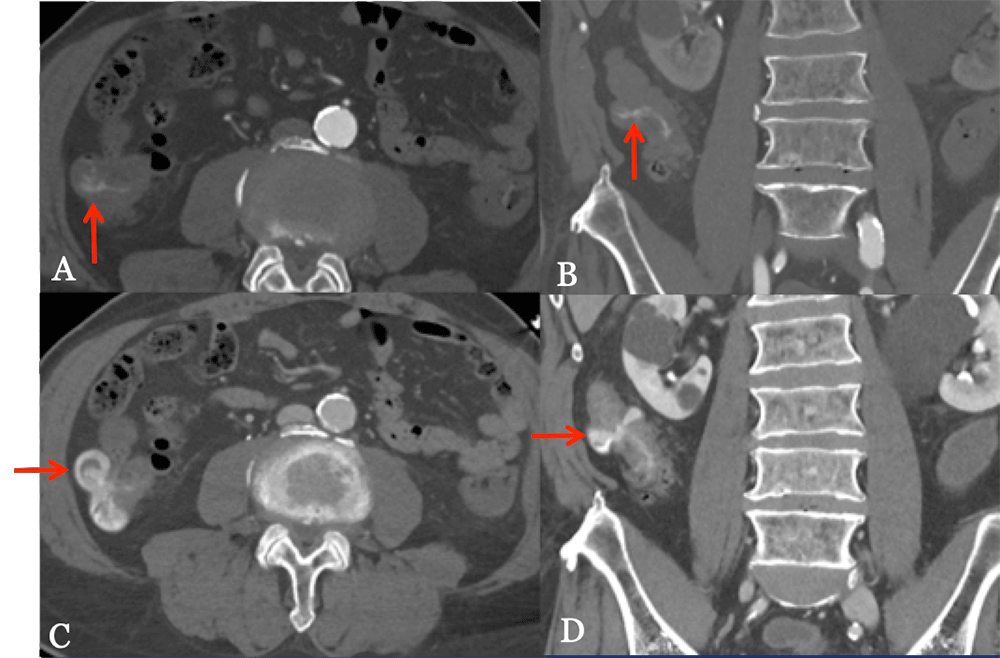 |
Refererences
|
Refererences
|
Refererences
|
Refererences
|
Refererences
|
