Computed Tomography of Superior Mesenteric Artery Syndrome: The Role of Multiplanar Reconstruction and 3D Imaging
Computed Tomography of Superior Mesenteric Artery Syndrome: The Role of Multiplanar Reconstruction and 3D Imaging Johns Hopkins Hospital The Russell H. Morgan Department of Radiology and Radiological Science |
Superior Mesenteric Artery (SMA) Syndrome 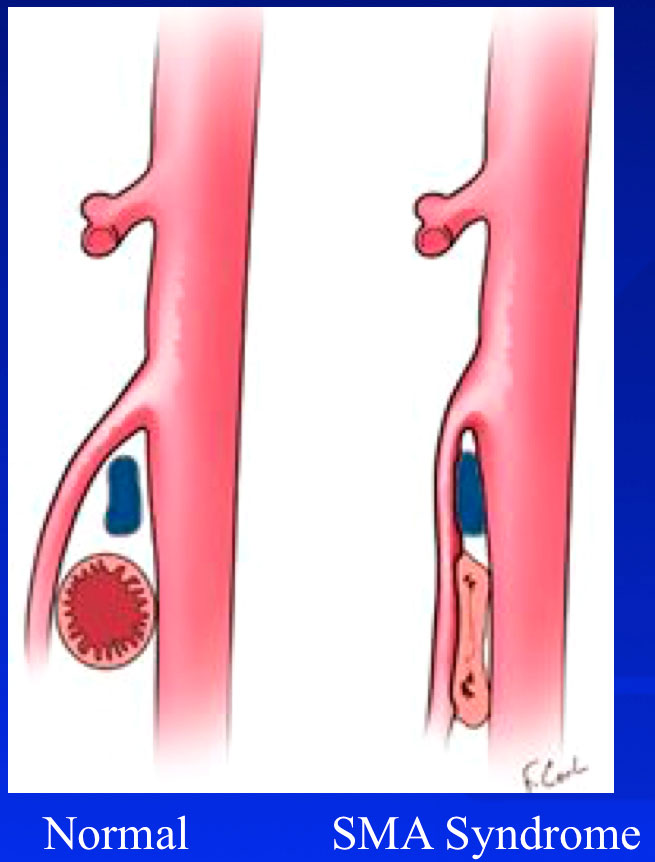 SMA syndrome is an uncommon but well recognized clinical entity characterized by compression of the third, or transverse, portion of the duodenum (D3) between the aorta and the superior mesenteric artery. Other terms used for this condition: - cast syndrome - Wilkie syndrome - arteriomesenteric duodenal obstruction - aortomesenteric artery compression - duodenal vascular compression - chronic duodenal ileus |
Typical Clinical History:
|
 Figure 1. 20 yo female with nausea, vomiting, and weight loss associated with meals. Mild nausea and epigastric discomfort began at age 14, with significant worsening and 30 pounds weight loss in the last few months. Duodenum is dilated in the 2nd and 3rd portion and compressed as it crosses beneath the SMA (axial image). Left gonadal vein is prominent. |
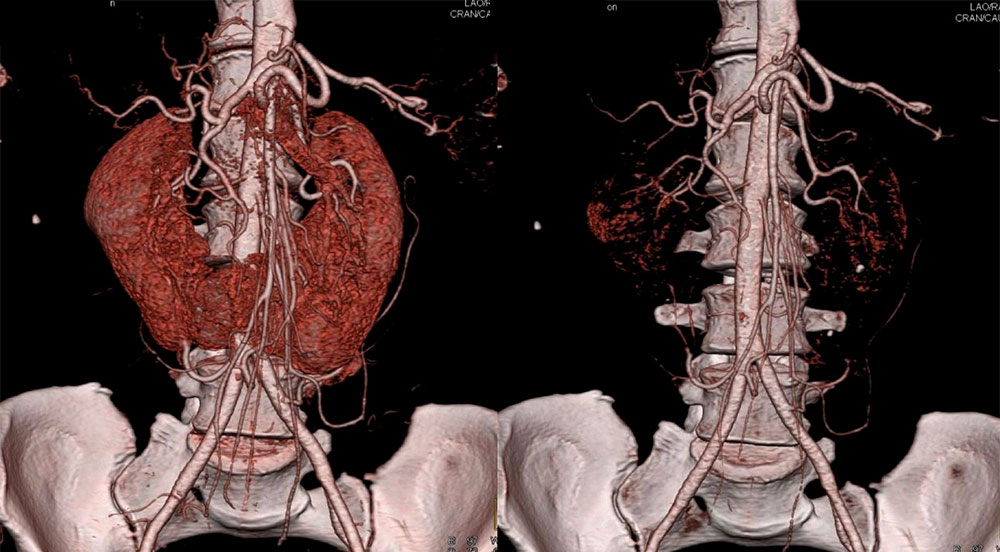 Figure 2. 48 yo female with 20 years of chronic abdominal pain, worse over last 6 months. After diagnosis of SMA syndrome, patient undergone side-to-side duodenojejunostomy with significant improvement. 3D images show dilated left renal vein and a horseshoe kidney. |
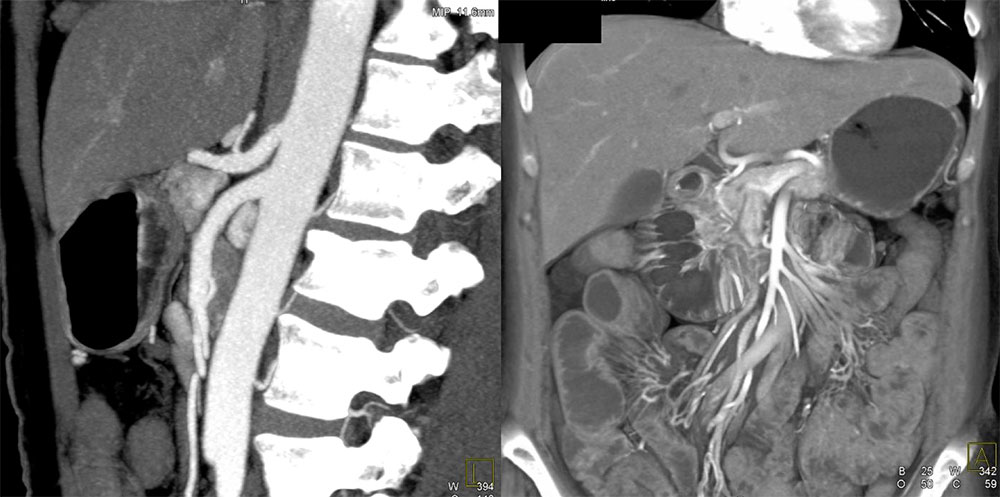 Figure 3A. 51 yo female with abdominal pain. Sagittal image demonstrates decreased aorta-SMA angle and distance. Distended stomach and proximal duodenum are well seen on volume rendering. |
 Figure 3B. Same patient. 3D reconstructions demonstrate prominent left renal vein until the point of crossing between aorta and SMA. IVC filter is seen on coronal image. |
 Figure 4A. 46-year-old female who has been completely disabled and incapacitated by persistent abdominal pain that is brought on by eating. SMA arises at a sharp angle with distance between the posterior aspect of the SMA and the ascending aorta of about 5 mm. After duodenojejunostomy patient was better able to eat and has gained weight |
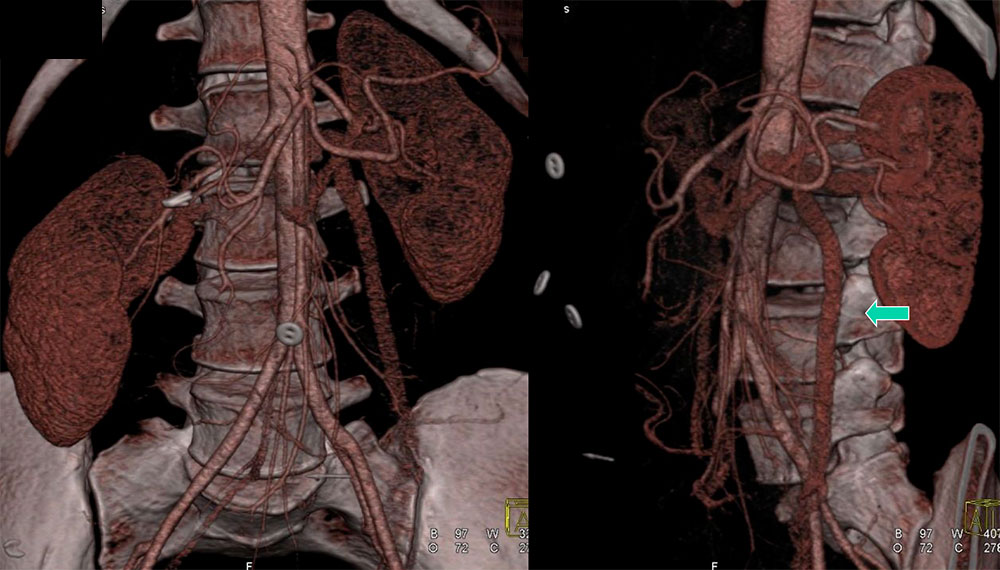 Figure 4B. Same patient. 3D reconstructions show dilated compressed left renal vein. Left gonadal vein is also prominent in size (arrow). |
Typical Clinical History:
|
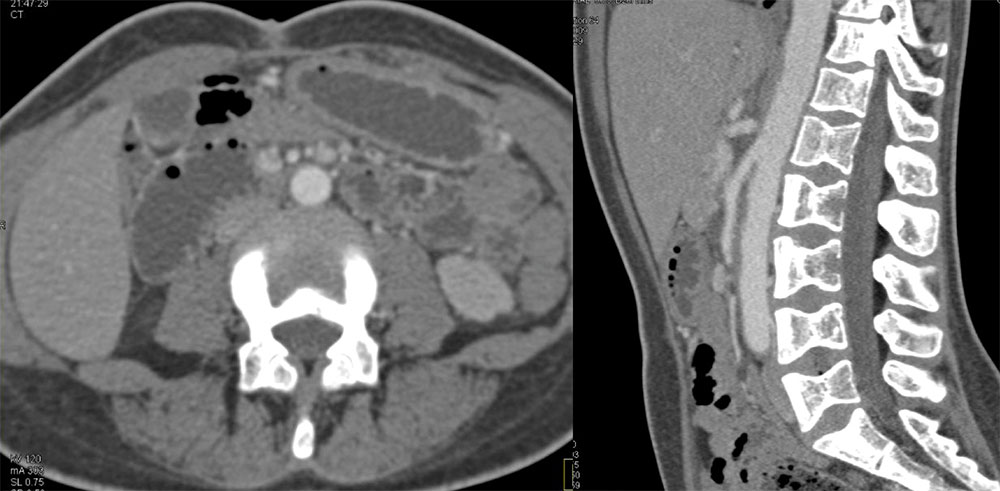 Figure 5. 26-year-old female with sickle cell disease, abdominal pain, vomiting, and nausea. Upper GI and endoscopy showed dilated proximal duodenum to the level of SMA. Delayed gastric emptying was seen on nuclear medicine study. Axial image shows dilated duodenum. Decreased aorta-SMA angle and distance are seen on sagittal image. |
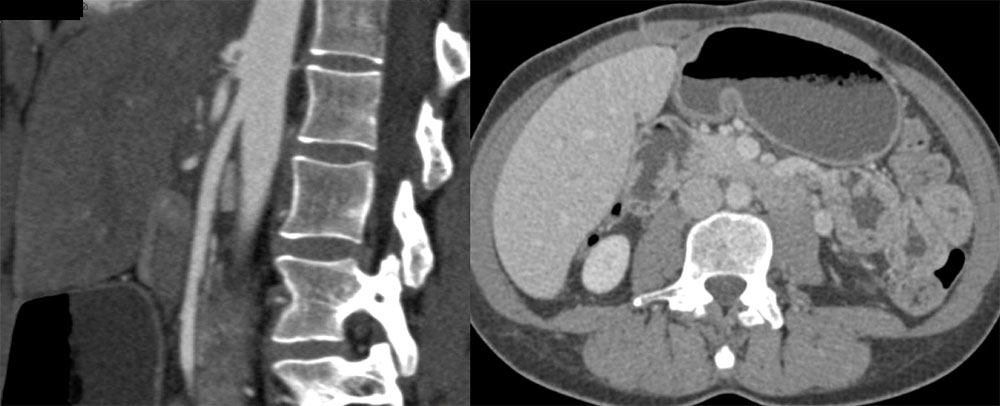 Figure 6A. 35-year-old female with intermittent, increasing episodes of nausea and vomiting dating back 6 years, some requiring ER visits and hospitalization. Five years ago patient had a laparoscopic cholecystectomy, as initially symptoms were attributed to the gallbladder problems. Sagittal image shows narrowing of the angle between the SMA and the aorta. Axial image shows dilated stomach and duodenum. |
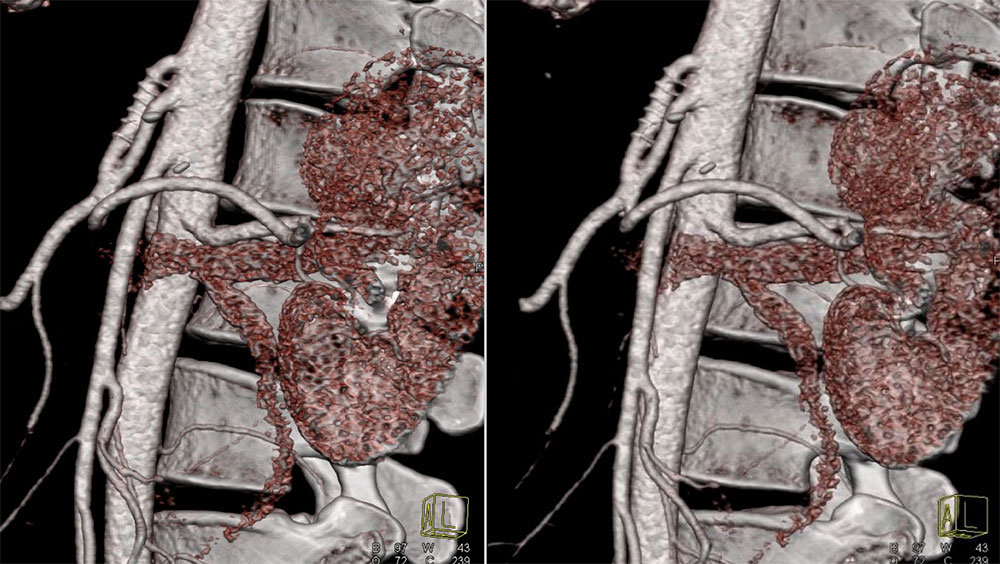 Figure 6B. Same patient. Patient was also diagnosed with a median arcuate ligament syndrome and underwent a celiac artery stenting about 5 years ago. After recent duodenojejunostomy patient reports some improvement. 3D images demonstrate celiac stent and small distance between SMA and the aorta. There is dilated left renal vein compressed behind the SMA, which is a common finding. |
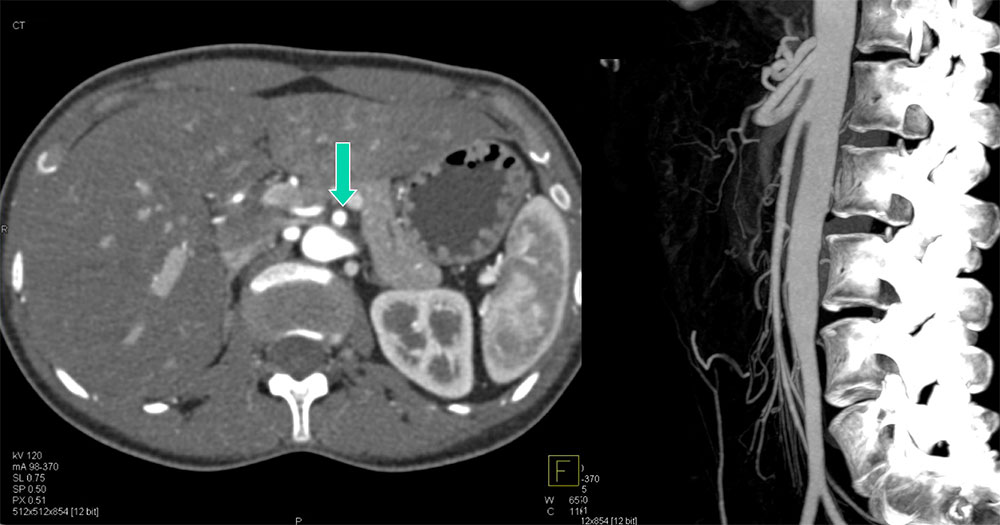 Figure 7A. 32 yo female with abdominal pain, progressive bloating, nausea, occasional emesis, and weight loss for two months . Her diet is now mainly is limited to liquids with trials of nutritional supplements. Distance between the SMA (arrow on axial images) and the aorta is markedly narrowed. |
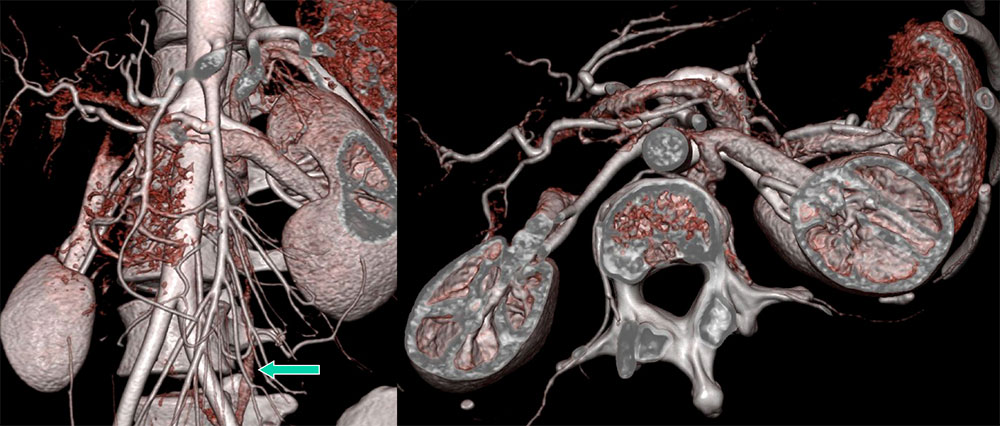 Figure 7B. Same patient. 3D images demonstrate compressed left renal vein and a prominent left lumbar collateral (arrow). Patient has undergone a laparoscopic duodenojejunostomy for SMA syndrome correction and now reports significant improvement in symptoms. |
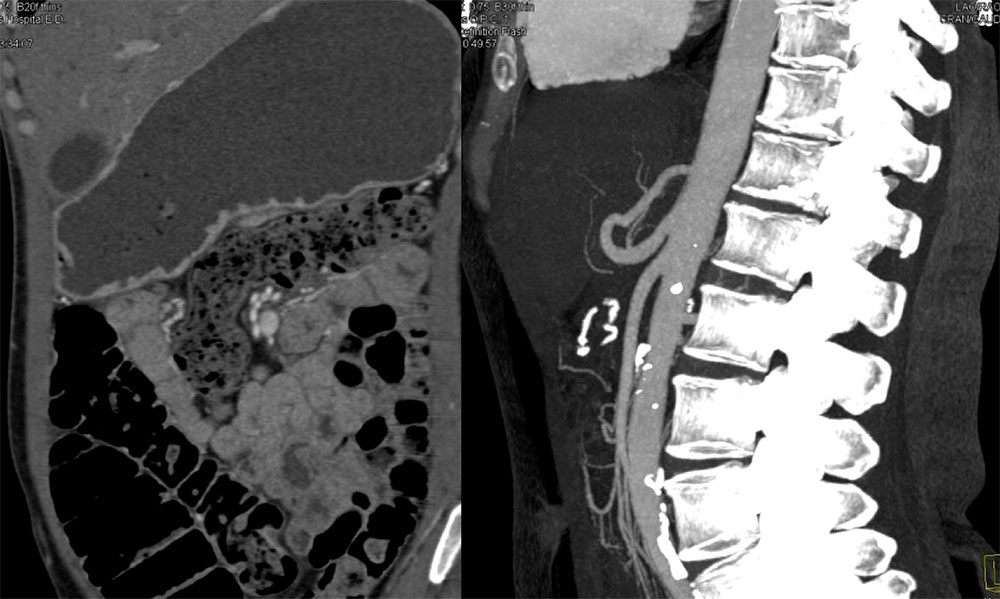 Figure 8A. 45-year-old female with 1-1/2-year history of progressively worsening abdominal symptoms. She describes worsening abdominal pain and bloating, especially with any food. Often she is actually afraid to eat food because of the pain. CT shows markedly distended stomach and narrowed aorta-SMA distance and angle. |
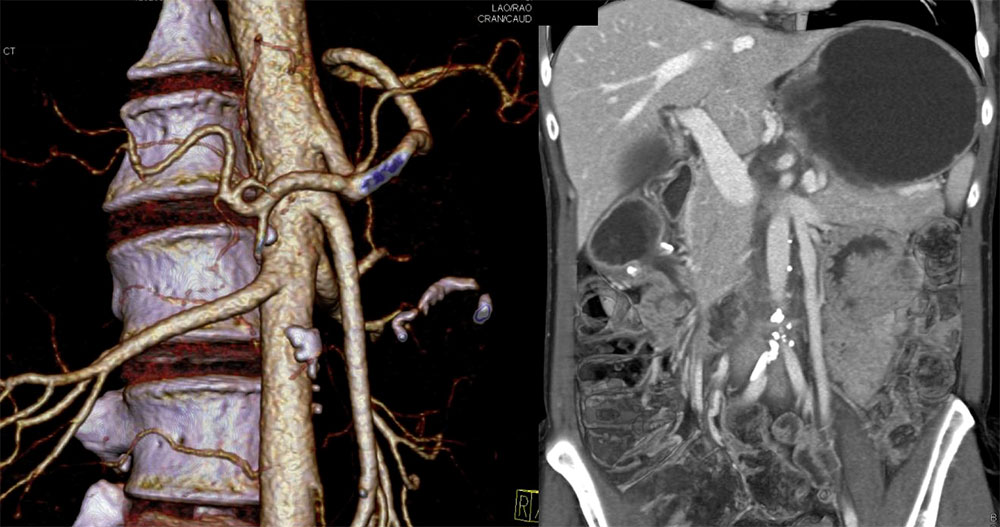 Figure 8B. Same patient. 3D images demonstrate distended stomach and some duodenum and narrowed aorta-SMA distance and angle. Patient undergone laparoscopic side-to-side gastrojejunostomy with significant improvement in symptoms. |
Typical Clinical History:
|
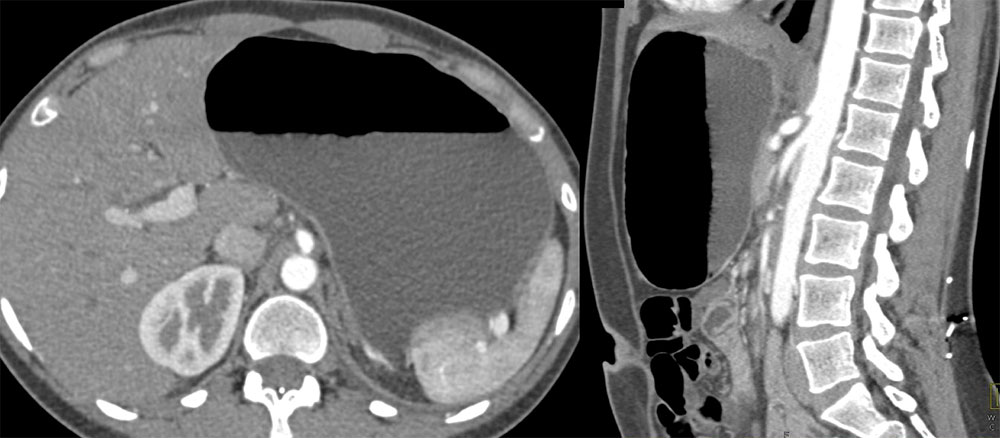 Figure 9A. 27 yo female with right lower quadrant pain and bloating. CT demonstrates a markedly distended stomach and decreased aorta-SMA angle and distance. |
 Figure 9B. Same patient. Volume rendering demonstrates distended stomach and proximal duodenum. There is small aorta-SMA angle and distance and some pinching of the left renal vein. |
SMA Syndrome Pathophysiology and Direct Radiologic Findings 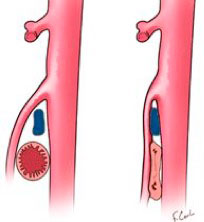
|
 Figure 10. Same patient as in figure 6. Sagittal image shows an example of measuring the angle between the SMA and the aorta. In this case the aorta-SMA angle is about 16°. |
Indirect Radiologic Signs Helpful on Axial Images If multiplanar or 3D reconstructions typically performed only after an analysis of the axial images, these indirect signs are helpful in deciding on further evaluation:
|
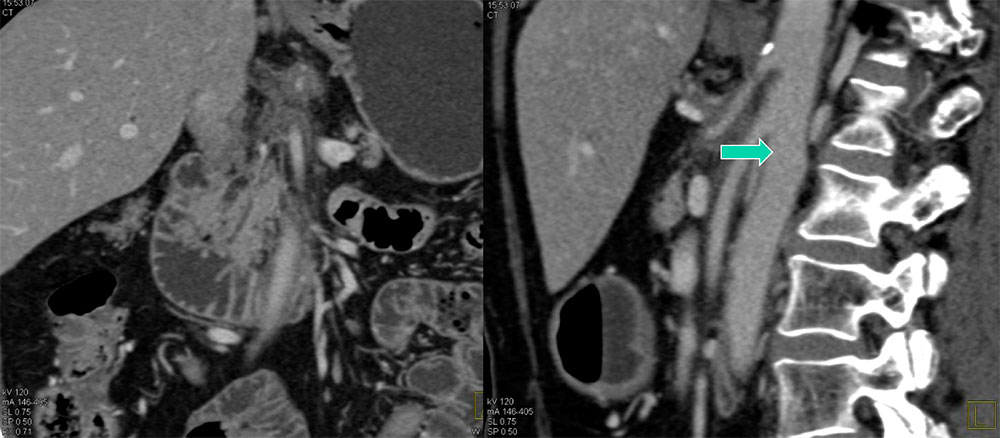 Figure 11. 67 yo female with right upper quadrant pain, weight loss and diarrhea for 6 months, worse with meals. Images show soft tissue encasement of the celiac and the SMA (arrow). Proximal duodenum is dilated. Endoscopic ultrasound revealed changes of chronic pancreatitis and this diagnosis was confirmed by other tests. Biopsies of the soft tissue around SMA did not reveal malignancy. |
Epidemiology of SMA syndrome:
|
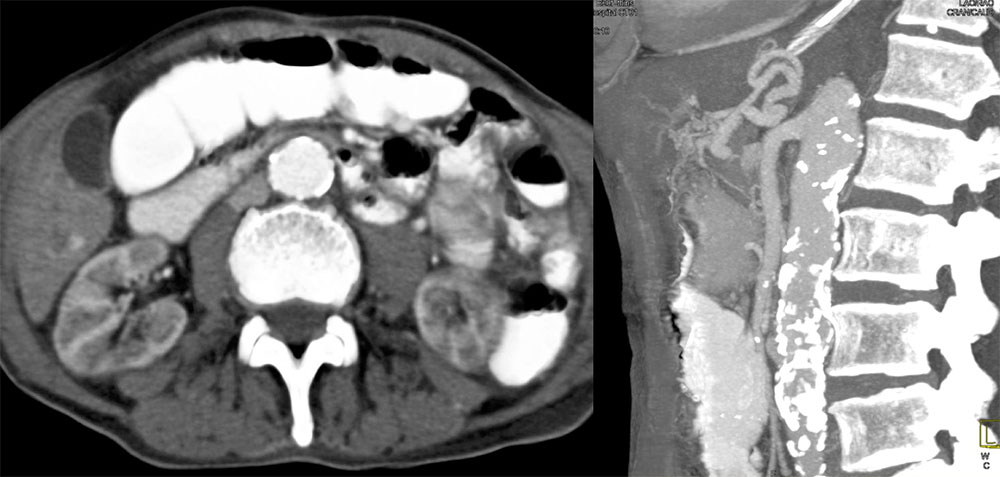 Figure 12. 76 yo male with abdominal pain. Duodenum is dilated in the 2nd and 3rd portion until the SMA (axial image). Although angle of the SMA origin is appropriate, atherosclerosis and tortuosity of the vessel created an area of narrowing between the SMA and aorta. |
Predisposing conditions:
|
Predisposing conditions:
|
 Figure 13A. 65 yo female with abdominal pain. There is a large necrotic mass in the head and neck of the pancreas. SMA angle and distance from SMA to aorta are markedly decreased. Common bile duct stent is seen. |
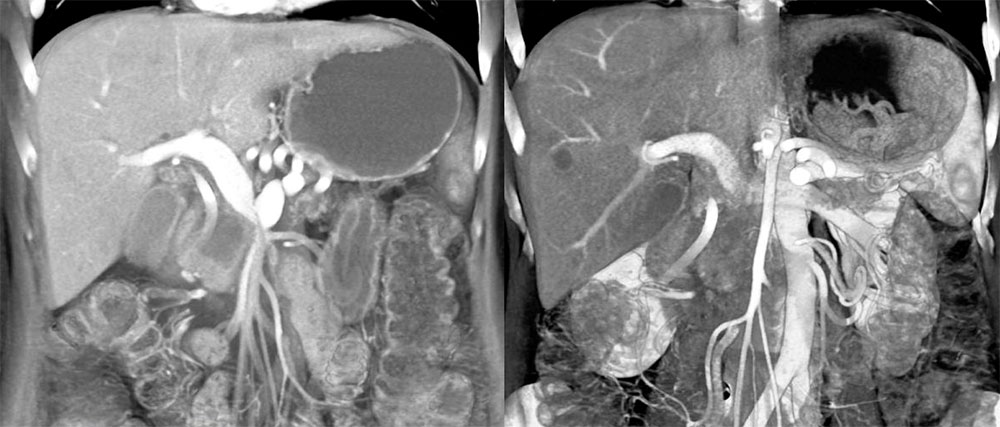 Figure 13B. Same patient. Volume rendering again demonstrates a large necrotic mass in the head and neck of the pancreas. Liver metastases and common bile duct stent are seen. Dilated left renal vein passing between aorta and SMA is also noted. |
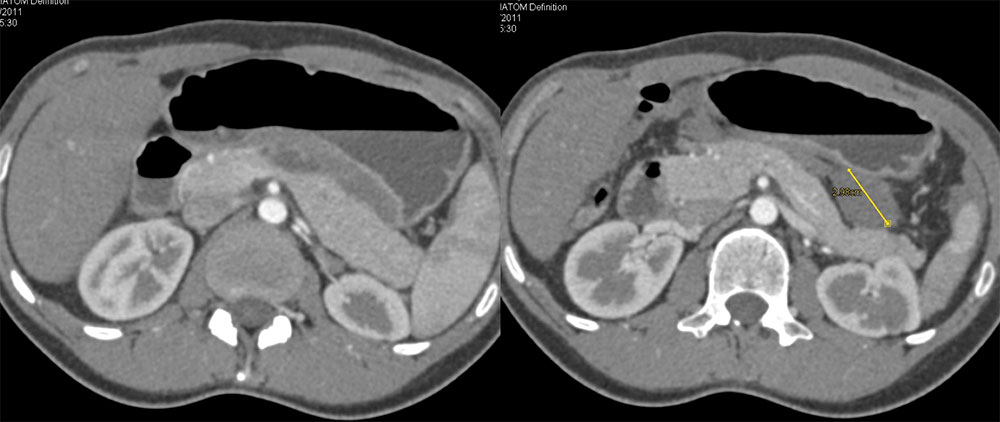 Figure 14A. 21 yo female with history of desmoid tumors. Axial images demonstrate distended stomach and duodenum. Desmoid tumor is delineated by calipers on the second image. |
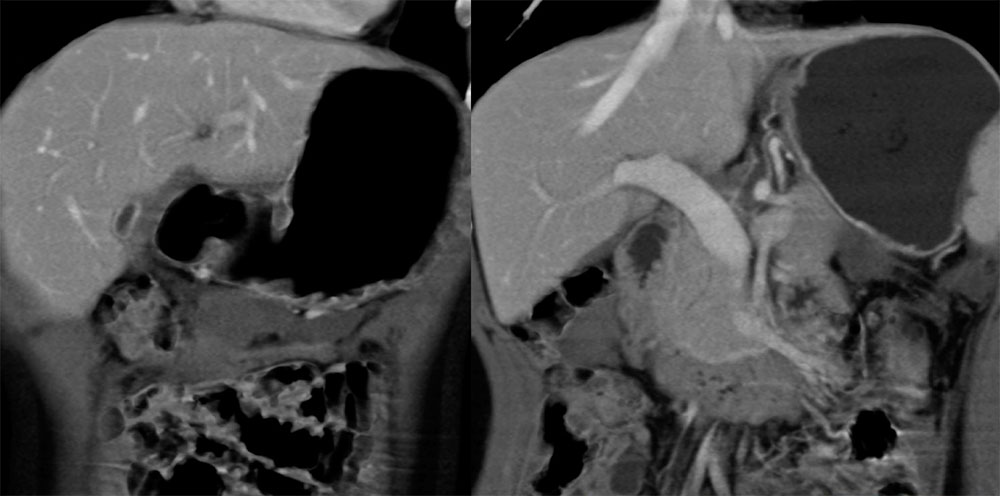 Figure 14B. Same patient. 3D images demonstrate distended stomach and duodenum. Bilateral cystic masses consistent with known desmoid tumors are again seen. |
Summary:
|
References:
|
