Case 9 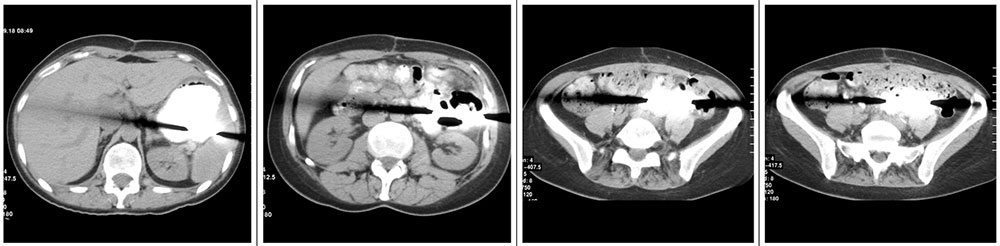 49 year old woman status post cytoreductive surgery 2 weeks prior. IV contrast enhanced CT shows:
|
Case 9 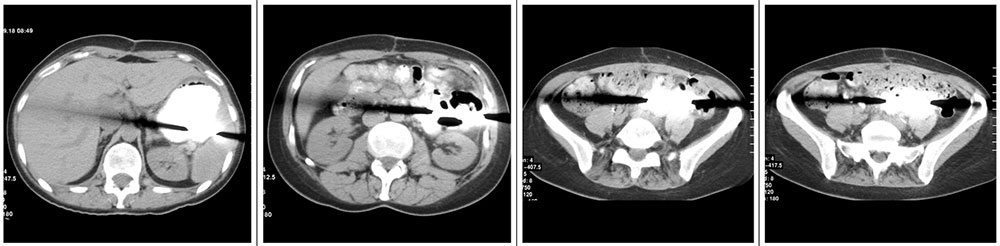 49 year old woman status post cytoreductive surgery 2 weeks prior. IV contrast enhanced CT shows:
|
Retained Metal Malleable Retractor 
|
Case 10  Chest radiograph on a 48 year old man shows:
|
Case 10  Chest radiograph on a 48 year old man shows:
|
Wireless capsule pH monitoring device 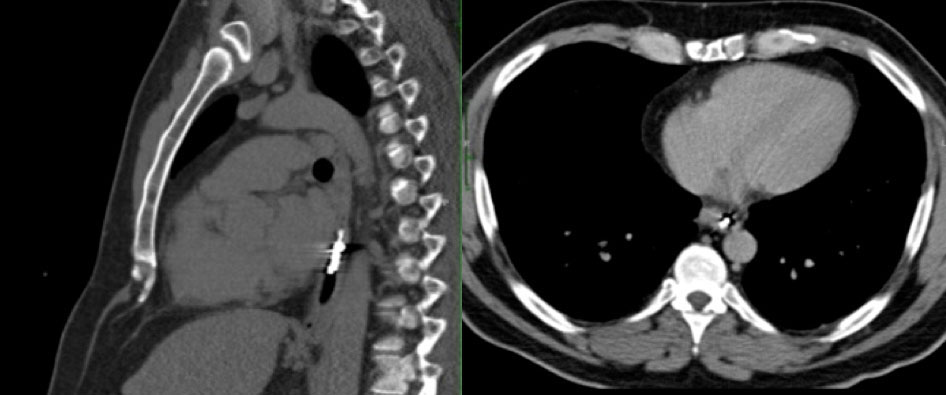
|
Case 11 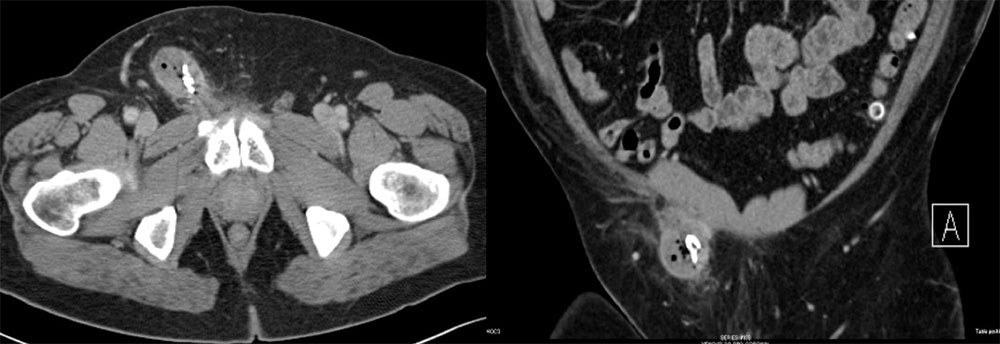 55-year-old man with a pancreatic mass and history of recent inguinal hernia repair. Axial (A) and coronal MPR (B) CT images of the pelvis reveal:
|
Case 11 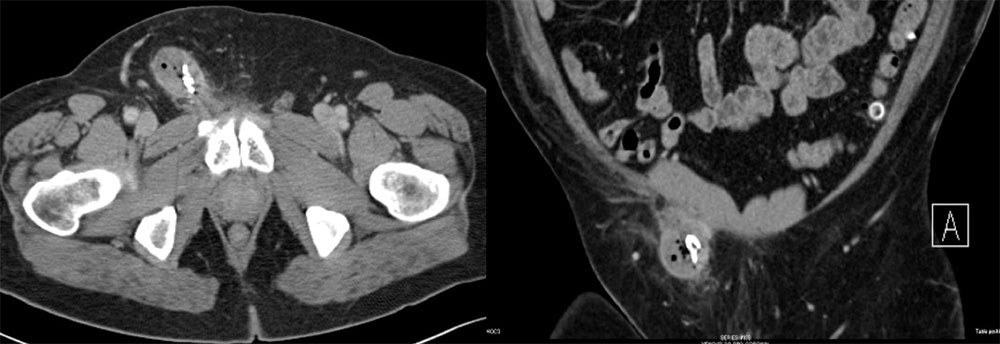 55-year-old man with a pancreatic mass and history of recent inguinal hernia repair. Axial (A) and coronal MPR (B) CT images of the pelvis reveal:
|
Retained Surgical Sponge
|
Retained Surgical Sponge 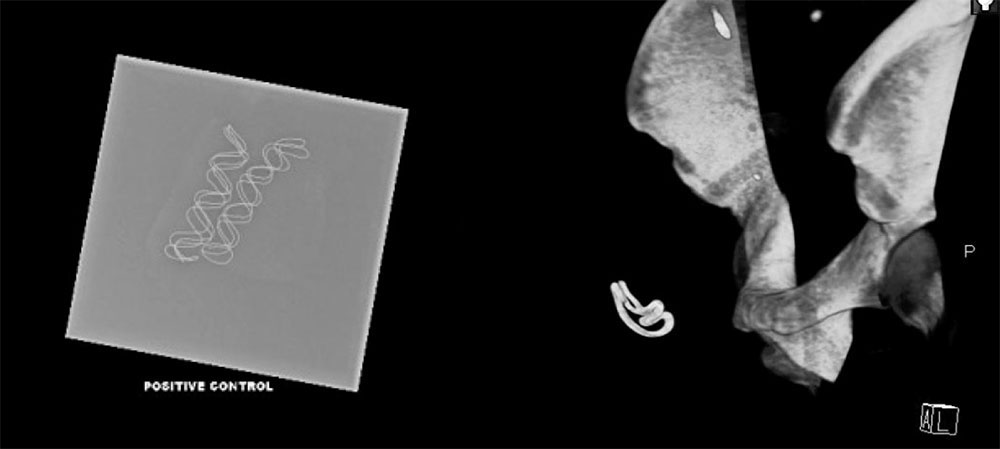 This is another example of how the sponge marker is better displayed with 3D volume rendering |
Case 12 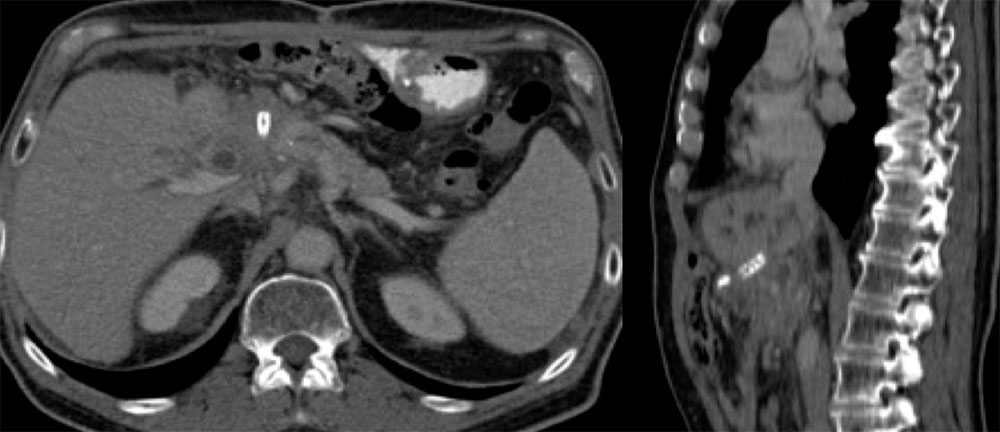 67 year old man w/ampullary adenocarcinoma, status post whipple complicated by gastroduodenal artery hemorrhage necessitating hepatic artery stent. CT performed for follow up showed interval increase in biliary obstruction, narrowing of the portal vein confluence, concerning for recurrent tumor Axial CT and sagittal MPR demonstrate:
|
Case 12 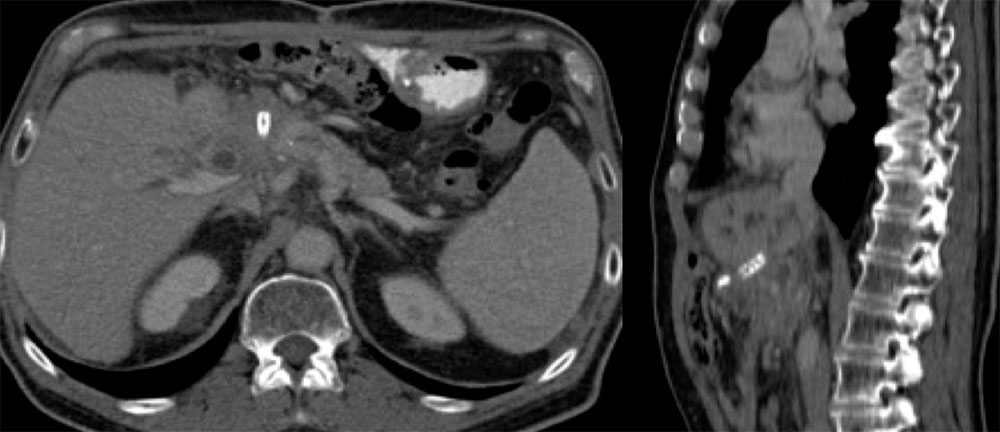 67 year old man w/ampullary adenocarcinoma, status post whipple complicated by gastroduodenal artery hemorrhage necessitating hepatic artery stent. CT performed for follow up showed interval increase in biliary obstruction, narrowing of the portal vein confluence, concerning for recurrent tumor Axial CT and sagittal MPR demonstrate:
|
Migrated Hepatic Artery Stent
|
Migrated Hepatic Artery Stent 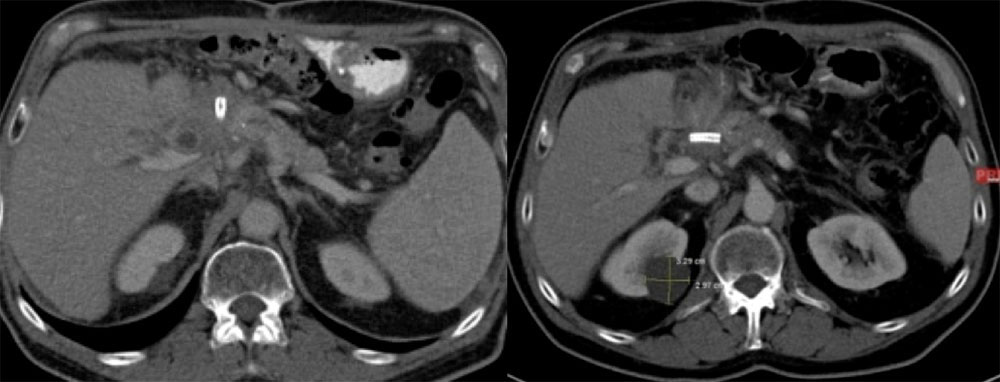
|
Case 13  Abdominal images on a 60 year old woman show small bowel obstruction and:
|
Case 13  Abdominal images on a 60 year old woman show small bowel obstruction and:
|
Retained Capsule Endoscopy 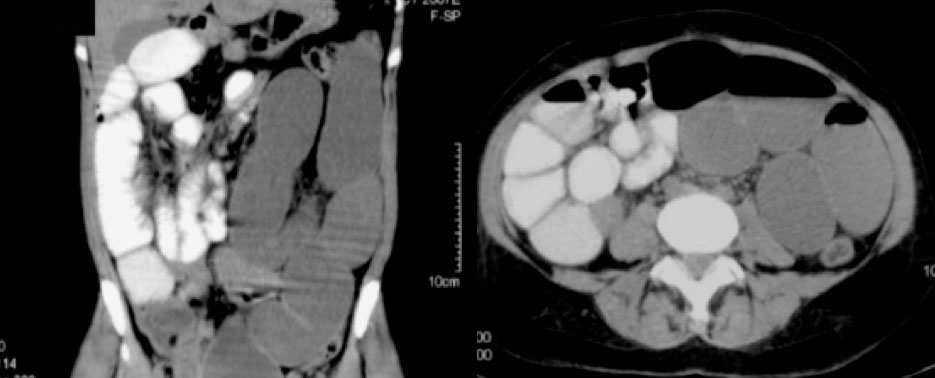
|
Retained Capsule Endoscopy
|
Case 14 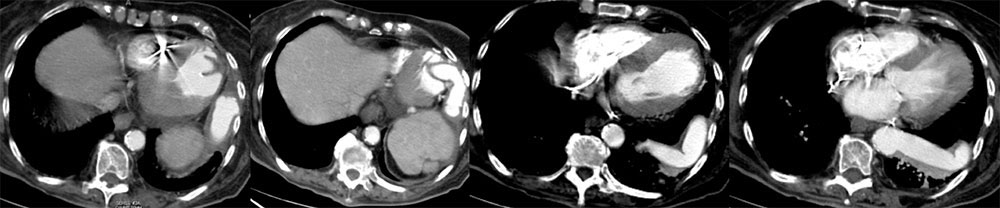 89 year old woman being imaged for melanoma staging. Axial IV contrast enhanced CT shows which of the following:
|
Case 14 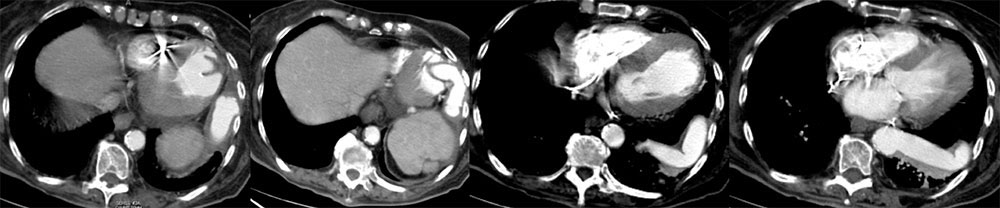 89 year old woman being imaged for melanoma staging. Axial IV contrast enhanced CT shows which of the following:
|
Apicoaortic Graft
|
Apicoaortic Graft
|
Case 15 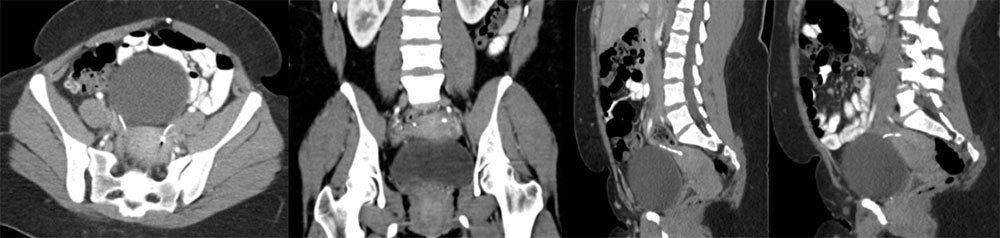 Axial image (A), coronal MPR (B), right sagittal oblique MPR (C) and left sagittal oblique MPR (D) from IV contrast enhanced CT of the pelvis demonstrate:
|
Case 15 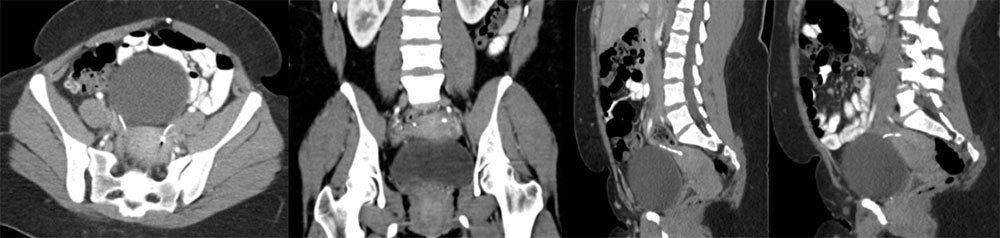 Axial image (A), coronal MPR (B), right sagittal oblique MPR (C) and left sagittal oblique MPR (D) from IV contrast enhanced CT of the pelvis demonstrate:
|
ESSURE Noninvasive Sterilization
|
ESSURE Noninvasive Sterilization
|
Intraoperative Radiography
|
Intraoperative Radiography
|
Intraoperative Radiography
|
Intraoperative Radiography
|
Intraoperative Radiography 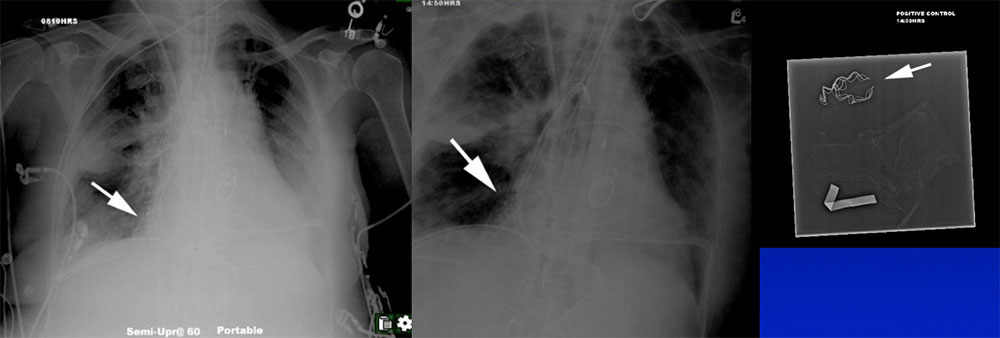 |
Intraoperative Radiography 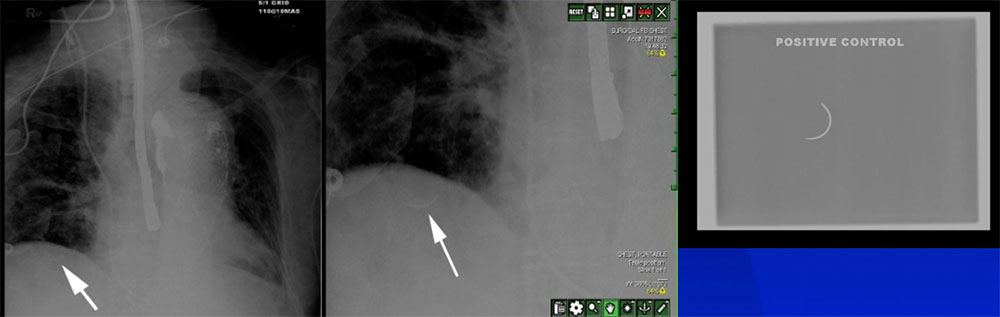 |
Conclusion
|
References
|

