|
-- OR -- |
|
- “ While radiation risk estimates at the low doses associated with CT contain considerable uncertainty, we choose to err on the side of safety by assuming a small risk exists, even though the risk at these dose levels may be zero.”
Perspective on radiation risk in CT imaging
Fletcher JG et al.
Abdom Imaging (2012)
DOI: 10.1007/s00261-012-9933-z - “ However, because the magnitude of net benefit is driven by the potential benefit of a positive exam, radiation dose should not be reduced if doing so may comprimise making an accurate diagnosis.”
Perspective on radiation risk in CT imaging
Fletcher JG et al.
Abdom Imaging (2012)
DOI: 10.1007/s00261-012-9933-z - “ However, because the magnitude of net benefit is driven by the potential benefit of a positive exam, radiation dose should not be reduced if doing so may comprimise making an accurate diagnosis. The benefits and risks of CT are also highly individualized, and require consideration of many factors by patients, clinicians and radiologists.”
Perspective on radiation risk in CT imaging
Fletcher JG et al.
Abdom Imaging (2012)
DOI: 10.1007/s00261-012-9933-z - Key Issues With Radiation Dose
- What parameters are we actually measuring when we list dose from a CT scan like the CT volume dose index (CTDIvol)?
- What are the risk/rewards of a CT scan for the individual patient at that point in time?
- What does past studies on radiation exposure (Hiroshima, nuclear workers, previously treated patients) really saw?
- How do we maintain science when journalism is involved? - CT and Radiation Dose in the News Media (NYT)




- Less than 48 hours later; 8-20-2012 vs 8-22-2012

- “ Compared with standard FBP reconstruction, an IRIS algorithm enables significant reduction of image noise and improvement of image quality and has the potential to decrease radiation exposure during contrast enhanced dual energy CT abdominal examinations.” Improved Image Quality in Dual Energy Abdominal CT: Comparison of Iterative Reconstruction in Image Space and Filtered Back Projection Reconstruction Wang R et al. AJR 2012; 199:402-406
- “ The image noise using IRIS algortihm was lower than that using standard FBP algorithm on the liver, aorta, and subcutaneous fat respectively. The signal-to-noise ratio and contrast to noise ration of images reconstructed with the IRIS algorithm also were significantly higher than those reconstructed with the FBP algorithm”
Improved Image Quality in Dual Energy Abdominal CT: Comparison of Iterative Reconstruction in Image Space and Filtered Back Projection Reconstruction
Wang R et al.
AJR 2012; 199:402-406
- “ No prospective epidemiologic study with nonirradiated control subjects has quantitatively demonstrated adverse effects of radiation at doses less than about 100 mSv.”
Radiation Risks of Medical Imaging: Separating Fact from Fantasy
Hendee WR, O’connor MK
Radiology 2012; 264:312-321 - “The authors support efforts such as Image Gently and Image Wisely to use only enough radiation to acquire needed diagnostic information.The authors believe in three principles: to keep radiation doses as low as reasonably achievable (or ALARA), to keep medical procedures as safe as reasonably achievable (or ASARA), and to keep medical benefits as reasonably achievable (or AHARA).”
Radiation Risks of Medical Imaging: Separating Fact from Fantasy
Hendee WR, O’connor MK
Radiology 2012; 264:312-321 - “ The authors support efforts such as Image Gently and Image Wisely to use only enough radiation to acquire needed diagnostic information.”
Radiation Risks of Medical Imaging: Separating Fact from Fantasy
Hendee WR, O’connor MK
Radiology 2012; 264:312-321 - “ The authors believe in three principles: to keep radiation doses as low as reasonably achievable (or ALARA), to keep medical procedures as safe as reasonably achievable (or ASARA), and to keep medical benefits as reasonably achievable (or AHARA).”
Radiation Risks of Medical Imaging: Separating Fact from Fantasy
Hendee WR, O’connor MK
Radiology 2012; 264:312-321
- “ Use of CT scans in children to deliver cumulative doses of about 50 mGy might almost triple the risk of leukaemia and doses of about 60 mGy might triple the risk of brain cancer.”
Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study
Pearce MS et al.
Lancet June 7, 2012
DOI:10.1016/S0140-6736(12)60815 - “ Use of CT scans in children to deliver cumulative doses of about 50 mGy might almost triple the risk of leukaemia and doses of about 60 mGy might triple the risk of brain cancer. Because these cancers are relatively rare, the cumulative absolute risks are small; in the 10 years after the first scan for patients younger than 10 years, one excess case of leukemia and one excess case of brain tumor per 10,000 head CT scans is estimated to occur.”
Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study
Pearce MS et al.
Lancet June 7, 2012
DOI:10.1016/S0140-6736(12)60815 - “ Nevertheless, although benefits might outweigh the small absolute risks, radiation doses from CT scans should be kept as low as possible and alternative procedures, which do not involve ionizing radiation, should be considered if appropriate.”
Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study
Pearce MS et al.
Lancet June 7, 2012
DOI:10.1016/S0140-6736(12)60815 - “ The immediate benefits of CT outweigh the long term risks in many settings and because of CT’s diagnostic accuracy and speed of scanning, notably removing the need for anaesthesia and sedation in young patients, it will remain in widespread practice for the foreseeable future.”
Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study
Pearce MS et al.
Lancet June 7, 2012
DOI:10.1016/S0140-6736(12)60815
- “ A simple step is to review existing CT protocols to ensure that radiation does are as low as reasonably possible. In addition to reducing the number of phases acquired and other high level changes, the user can adjust the radiation output of the CT scanner through four scan parameters (kVp, mA, table speed cm/s, gantry rotation time).”
CT Radiation Dose: What Can You Do Right Now in Your Practice?
Coakley FV et al
AJR 2011; 196:619-625 - “ Excessively high mAs or kVp comments yielded sensitivity of only 21.2% in predicting examinations above the CTDIw DRLs, with a specificity of 87.6%. Using the 2008 CTDIvol DRLs, the corresponding sensitivity was 13.1% and specificity was 86.2%. Significance was not achieved for use of clinical parameters in predicting either CTDIw or CTDIvol.”
Can Experienced CT Radiologists Use Technique Parameters to Predict Excessive Patient Dose? An Analysis of the ACR CT Accreditation Database
Zeman RK et al.
J Am Coll Radiol 2011;8:275-280 - “ The aim of this study was to determine, for 3 basic clinical examinations, whether blinded, experienced CT radiologists participating in the ACRs CT Accreditation Program could use scan parameters such as tube current time (mAs), tube voltage (kVp), and pitch to predict scanner output settings, expressed as CTDIw and CTDIvol, exceeding CTDIw diagnostic reference levels (DRLs) set by the ACR in 2002 and CTDIvol DRLs adopted by the ACR in 2008.”
Can Experienced CT Radiologists Use Technique Parameters to Predict Excessive Patient Dose? An Analysis of the ACR CT Accreditation Database
Zeman RK et al.
J Am Coll Radiol 2011;8:275-280 - “ Experienced CT radiologists cannot reliably use scan parameters to predict examinations that exceed CTDIw or CTDIvol DRLs.”
Can Experienced CT Radiologists Use Technique Parameters to Predict Excessive Patient Dose? An Analysis of the ACR CT Accreditation Database
Zeman RK et al.
J Am Coll Radiol 2011;8:275-280 - “ CTDI cannot be used as a surrogate for patient dose, either in epidemiologic assessments of potential late effects or for potential deterministic effects (eg, skin injury). Neither CTDI nor its derivative, dose length product (DLP, which is the product of CTDI and the irradiated scan length) should be used to estimate effective dose or potential cancer risk for any individual patient.”
CT Dose Index and Patient Dose: They Are Not the Same Thing
McCollough CH et al.
Radiology 2011; 259:311-316 - “ CTDI provides a very useful way to compare the doses delivered by various scan protocols or to achieve a specific level of image quality for a specific size patient.”
CT Dose Index and Patient Dose: They Are Not the Same Thing
McCollough CH et al.
Radiology 2011; 259:311-316 - “ Estimates of individual patient risk, and epidemiologic studies assessing potential late effects, must use patient size-specific dose estimates-they cannot use only scanner output (CTDI or DLP). Rather use of the known exponential relationship between patient size and absorbed dose will allow patient size specific dose estimates to be made from scanner output values.”
CT Dose Index and Patient Dose: They Are Not the Same Thing
McCollough CH et al.
Radiology 2011; 259:311-316 - “ The CTDI is a standardized measure of the radiation output of a CT system, measured in a cylindrical acrylic phantom, that enables users to guage the amount of emitted radiation and compare the radiation output between different scan protocols or scanners. Complex calculations are required to map scanner output to patient dose, taking into account the patients size , irradiated organs, body composition, and scan range.”
CT Dose Index and Patient Dose: They Are Not the Same Thing
McCollough CH et al.
Radiology 2011; 259:311-316 - “ The CTDI is a standardized measure of the radiation output of a CT system, measured in a cylindrical acrylic phantom, that enables users to guage the amount of emitted radiation and compare the radiation output between different scan protocols or scanners.”
CT Dose Index and Patient Dose: They Are Not the Same Thing
McCollough CH et al.
Radiology 2011; 259:311-316 - “ The CTDI values are included in either a screen captured “patient dose report” or a structured Digital Imaging and Communications in Medicine dose report, which reinforces the incorrect belief that CTDI is a measure of patient dose.”
CT Dose Index and Patient Dose: They Are Not the Same Thing
McCollough CH et al.
Radiology 2011; 259:311-316 - “ Instead because the volume CTDI is displayed on the scanner console before the initiation of a scan ( to allow the operator to confirm that the proper scanner output is programmed) and recorded as part of the patients examination information, many users incorrectly assume that it is the dose to that particular patient.”
CT Dose Index and Patient Dose: They Are Not the Same Thing
McCollough CH et al.
Radiology 2011; 259:311-316 - “ Media reports often transform scientific concerns into facts, and the sensationalized reporting of a few radiation overdoses has catalyzed public unease, regulatory scrutiny, and legislative interest.”
Fears, Feelings, and Facts; Interactively Communicating Benefits and Risks of Medical Radiation with Patients
Dauer LT et al.
AJR 2011; 196:756-761 - “ The confluence of these concepts has triggered a classic media driven social amplification of the perceived seriousness of an accident or normal clinical practice. This can result in the stigmatization of radiation in medicine, which may result in a loss of public confidence and reluctance of patients to undergo necessary examinations or treatments.”
Fears, Feelings, and Facts; Interactively Communicating Benefits and Risks of Medical Radiation with Patients
Dauer LT et al.
AJR 2011; 196:756-761 - “ Radiogenic cancers are a late statistical risk because of the latent period of years to decades between irradiation and clinical cancer. There is no radiogenic risk if the patient does not survive long enough to manifest the cancer.”
Radiation Is Not the Only Risk
Balter S et al.
AJR 2011; 196:762-767 - “ Selecting the optimum procedure for an individual patient requires consideration of many factors of behefit and risk. Too much attention to radiogenic risk may distract attention from other risks and potential benefits. This may not be in the patients best interest.”
Radiation Is Not the Only Risk
Balter S et al.
AJR 2011; 196:762-767 "Thirty three percent of patients underwent five or more lifetime CT examinations, and 5% underwent between 22 and 132 examinations. Fifteen percent received estimated cumulative doses of more than 100 mSv, and 4% received between 250 and 1375 mSv. Associated LAR had mean and maximum values of 0.3% and 12% for cancer incidence and 0.2% and 6.8% for cancer mortality respectively."
Recurrent CT, Cumulative Radiation Exposure, and Associated Radiation-induced Cancer Risks from CT of Adults
Sodickson A et al.
Radiology 2009; 251:175-184"While most patients accrue low radiation-induced cancer risks from cumulative CT exposures, incremental risks are estimated to exceed 1% above baseline in 7% of scanned patients."
Recurrent CT, Cumulative Radiation Exposure, and Associated Radiation-induced Cancer Risks from CT of Adults
Sodickson A et al.
Radiology 2009; 251:175-184"Cumulative CT radiation exposure added incrementally to baseline cancer risk in the cohort. While most patients accrue low radiation-induced cancer risks, a subgroup is potentially at higher risk due to recurrent CT Imaging."
Recurrent CT, Cumulative Radiation Exposure, and Associated Radiation-induced Cancer Risks from CT of Adults
Sodickson A et al.
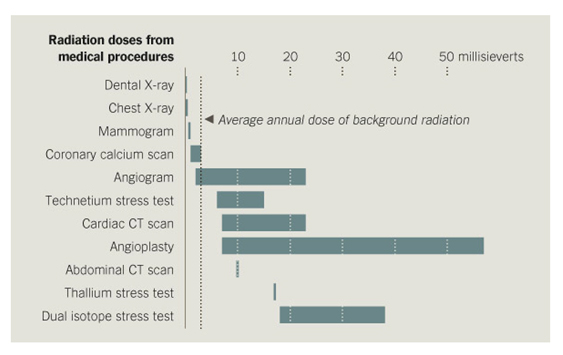
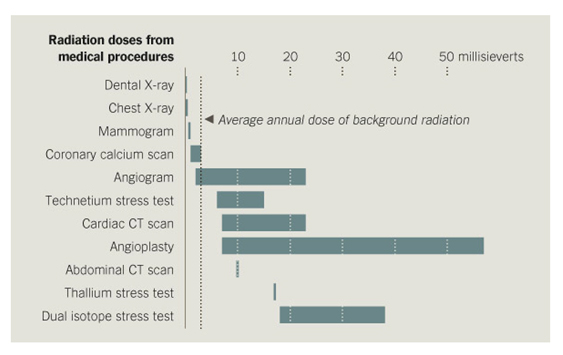
Radiology 2009; 251:175-184- Effective Doses of Select Radiologic Exams
The Case in Favor of Screening for Coronary Artery Disease With Coronary CT Angiography
Dowe DA
J Am Coll Radiol 2007;4:289-294
Head CT 1-2 mSv Chest CT 5-7 mSv Abdominal and pelvic CT 8-11 mSv Diagnostic Coronary Angiogram 3-30 mSv SPECT thallium stress test 25 mSv SPECT sestamibi stress test 12-18 mSv Retrospective gated CCTA 6-18 mSv Prospective Gated CCTA 1-8 mSv