CT of Calyceal Abnormalities in the Kidney: Pearls and Pitfalls
CT of Calyceal Abnormalities in the Kidney: Pearls and Pitfalls Elliot K. Fishman MD FACR Satomi Kawamoto MD Johns Hopkins Hospital |
Introduction
|
Normal Anatomy of Renal Collecting System 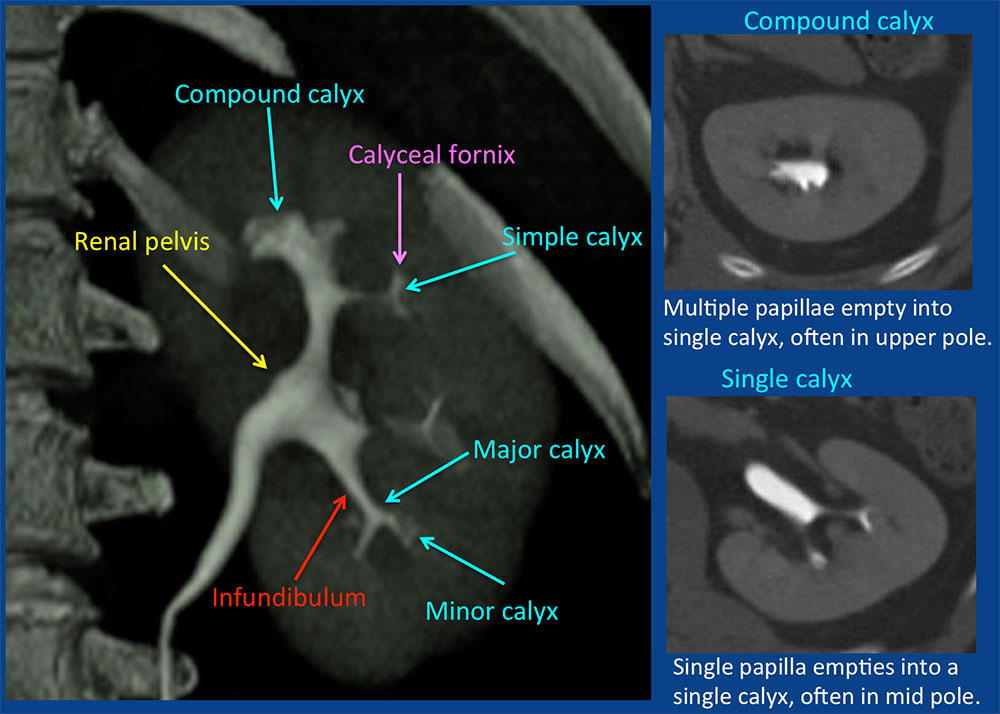 |
Prominent normal papilla 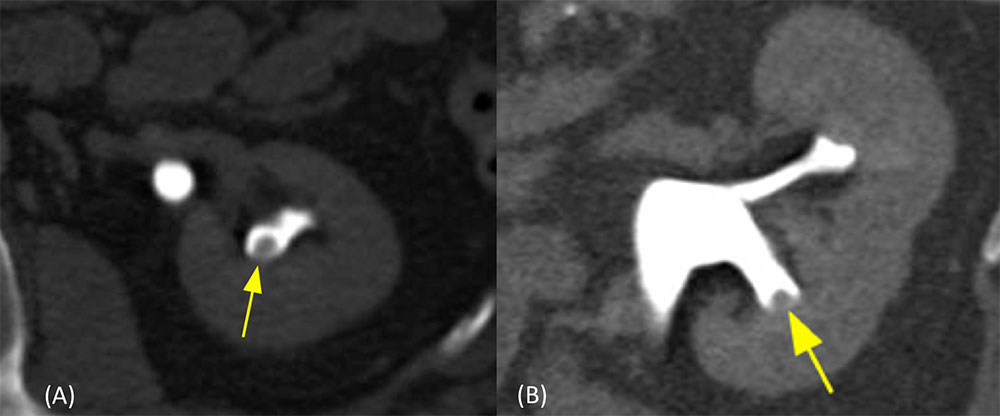 (A) Excretory phase axial CT image shows prominent normal papilla (arrow) which may simulate a polypoid mass. It should not be mistaken for urothelial lesion. (B) Excretory phase oblique sagittal CT image. Diagnosis of normal papilla can be confirmed by viewing in orthogonal planes by its central location within the calyx and smooth contour. |
Normal Papillary Blush 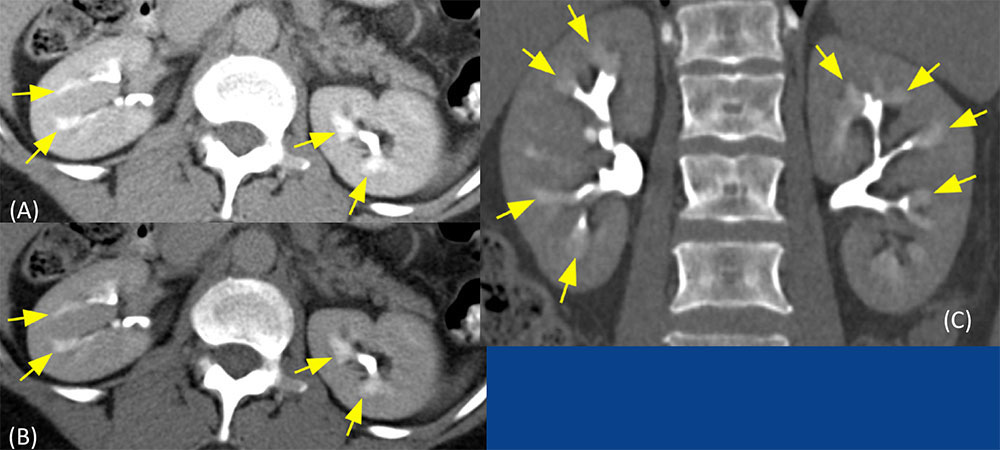 Normal papillary blush is accentuated with low-osmolality contrast media (less fluid is excreted into the tubular lumen, therefore the concentration of contrast material is higher than that with high-osmolality contrast material). Normal papillary blush in an asymptomatic patient. “blushlike” appearance (arrows), representing normal concentration of contrast in the medulla. |
Benign Tubular Ectasia 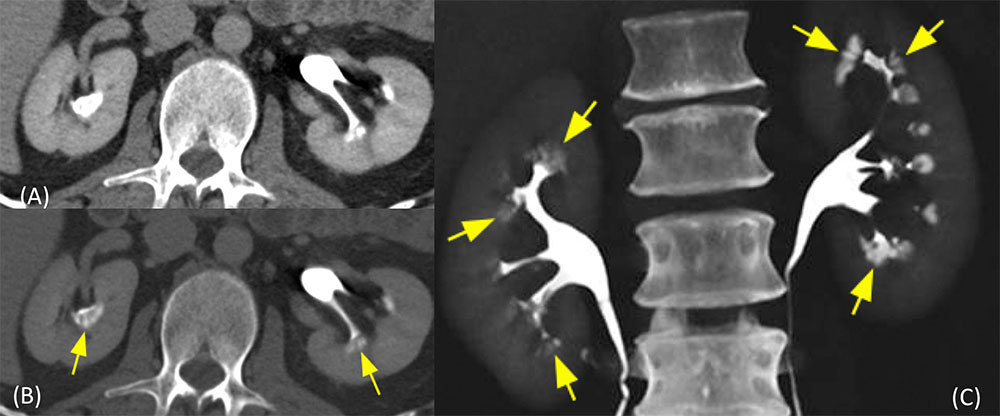 55-year-old man with benign tubular ectasia, presented with microscopic hematuria. (A, B) Excretory phase axial images and (C) coronal maximum intensity projection (MIP) image CT image show distinct, linear, “paintbrush”-like collections of contrast (arrows) in the dilated collecting ducts in the renal pyramids, which are difficult to appreciate on soft tissue window image (A), and better appreciated in wide window image (B) and coronal MIP image (C). |
Benign Tubular Ectasia/Medullary Sponge Kidney
|
Medullary Sponge Kidney (1) 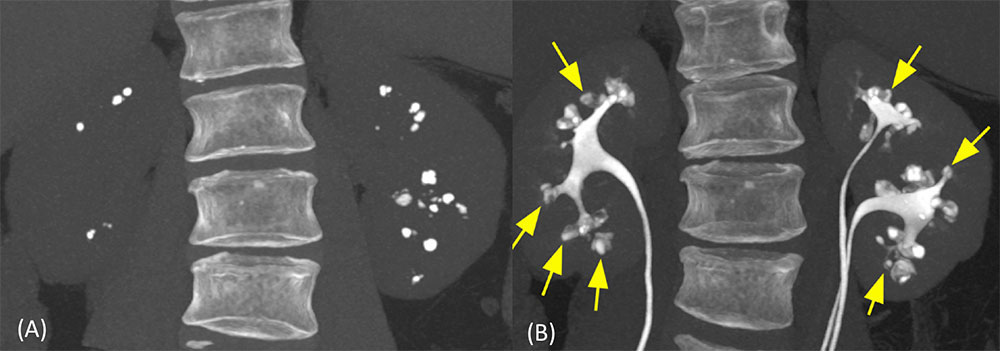 48-year-old man with history of urinary tract infection (UTI) and gross hematuria. History of Beckwith-Wiedemann Syndrome. (A) Noncontrast coronal MIP CT image shows extensive small and large calcifications in the medulla. (B) Excretory phase coronal MIP image shows calcifications are located in dilated collecting ducts. Additional densities (yellow arrows) are due to accumulation of contrast material within cystically dilated collecting ducts that do not already contain calculi.
|
Medullary Sponge Kidney (2) 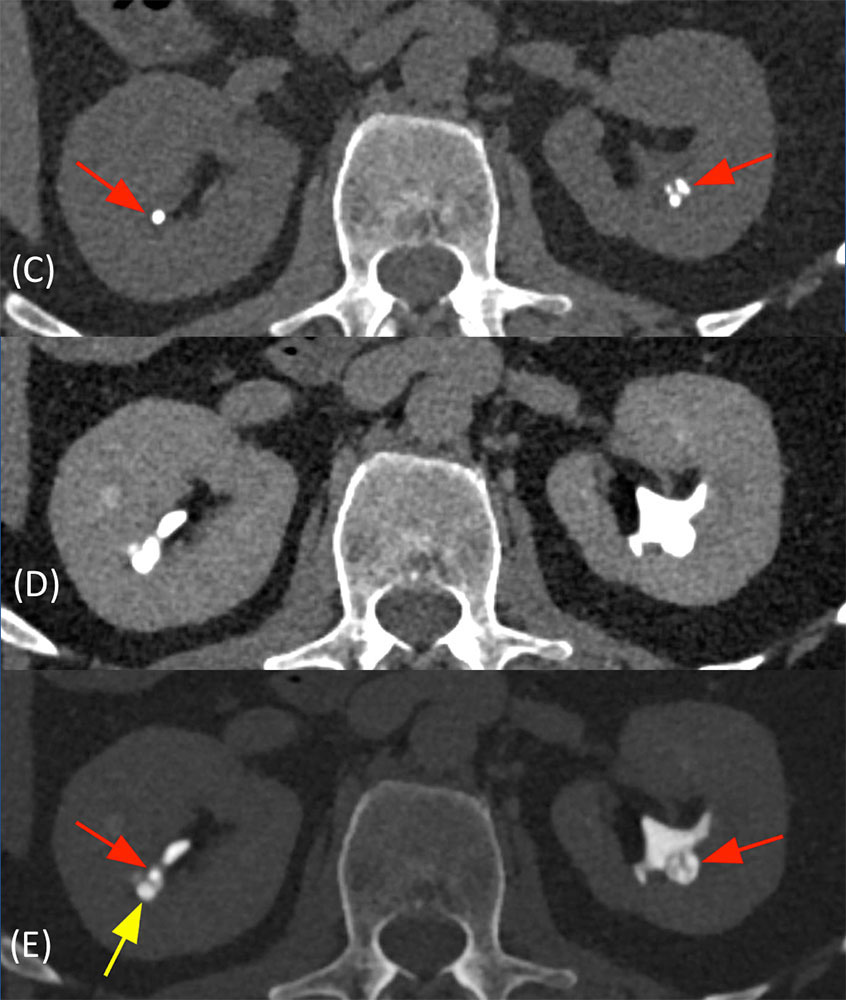 48-year-old man with history of UTI and gross hematuria. History of Beckwith-Wiedemann syndrome (Continuation from prior slide). (C) Noncontrast axial CT shows medullary nephrocalcinosis in the bilateral kidneys (red arrows). (D) On soft tissue window excretory phase CT, calcifications and dilatation of collecting ducts are obscured. (E) On wide window excretory phase CT, calcifications are located in dilated collecting ducts (red arrows). Additional density (yellow arrow) is due to accumulation of contrast material within cystically dilated collecting ducts that do not already contain calculus. In many patients with medullary sponge kidney, the affected collecting ducts are ectatic rather than cytically dilated. |
Medullary Nephrocalcinosis
|
Medullary Nephrocalcinosis 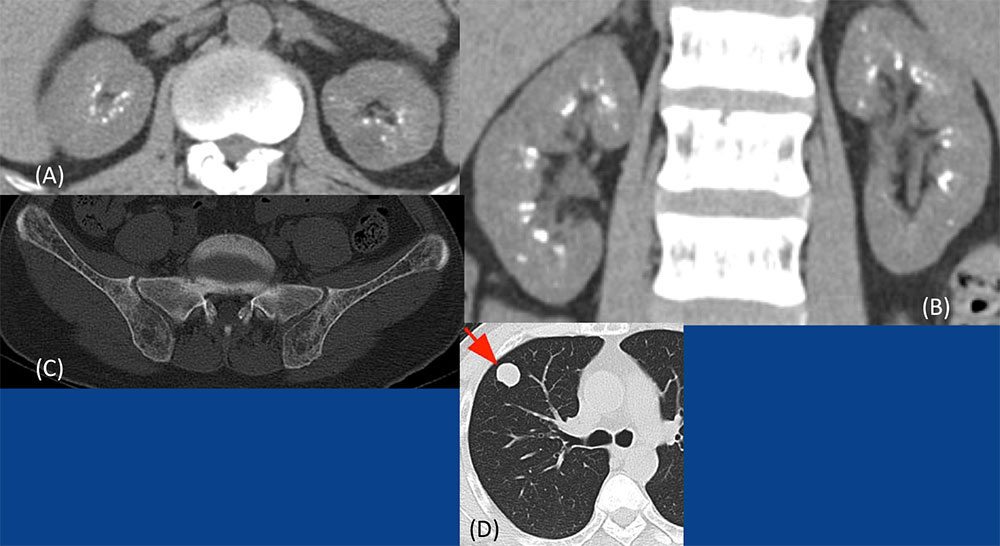 40-year-old male with prior resection of parathyroid carcinoma, presented with lung metastases and recurrent hyperparathyroidism. (A) Axial and (B) coronal noncontrast CT show multiple calcifications in the medulla. (C) Diffuse demineralization of pelvic bones. (D, E) Lung metastasis (arrow). Parathyroid carcinoma is less than 1% of all causes of hyperpara-thyroidism. |
Medullary Nephrocalcinosis 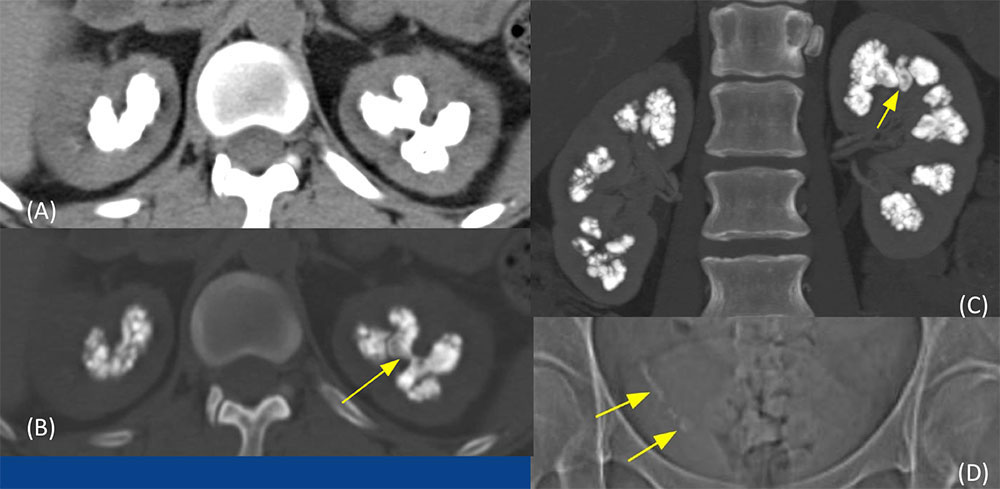 40-year-old woman with renal tubular acidosis type 1 (distal). History of renal stones, recurrent UTIs, presented with right flank pain. (A) Noncontrast axial soft tissue window and (B) wide window images, and (C) coronal postcontrast MIP image show massive calcifications in the renal medulla. A calculus fills the upper pole calyx (yellow arrow) is also seen (B, C). (D) Scout image shows multiple calculi in the distal right ureter (yellow arrows). Renal tubular acidosis Type 1 (distal): When massive medullary nephrocalcinosis is seen, renal tubular acidosis is usually the underlying cause. |
Urothelial Neoplasm
|
Urothelial Carcinoma 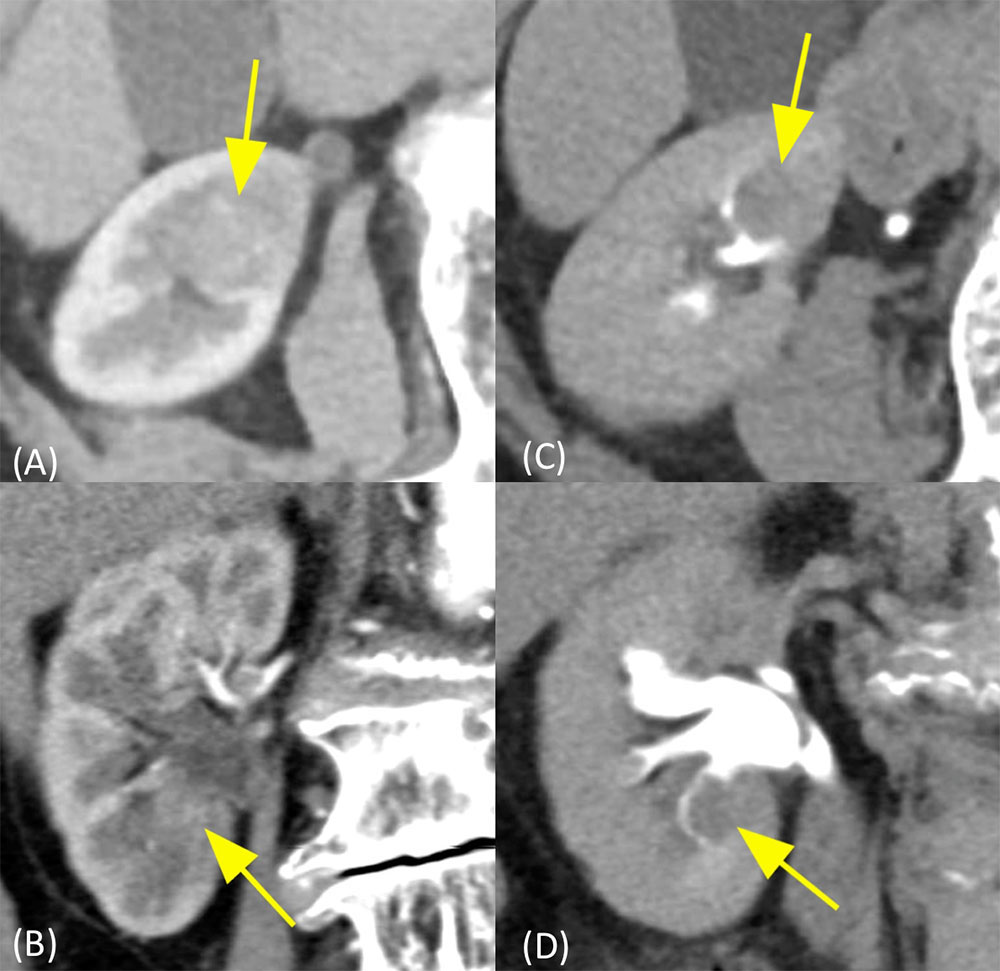 89-year-old woman presented to emergency room for gross painless hematuria. Pathology revealed high grade urothelial carcinoma which invaded deeply into the renal cortex to within 2 mm of the renal capsule (pT3). |
Multifocal Urothelial Carcinomas 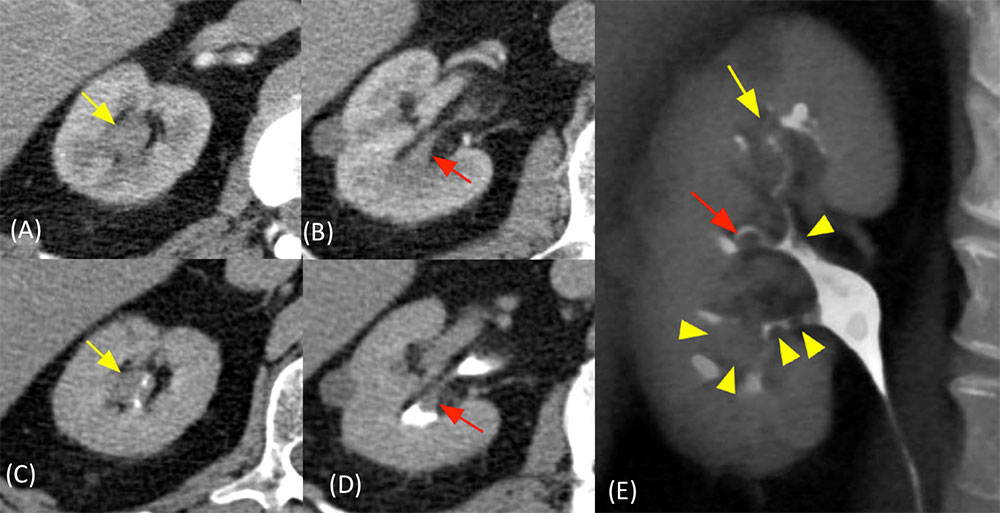 |
Medullary Nephrocalcinosis 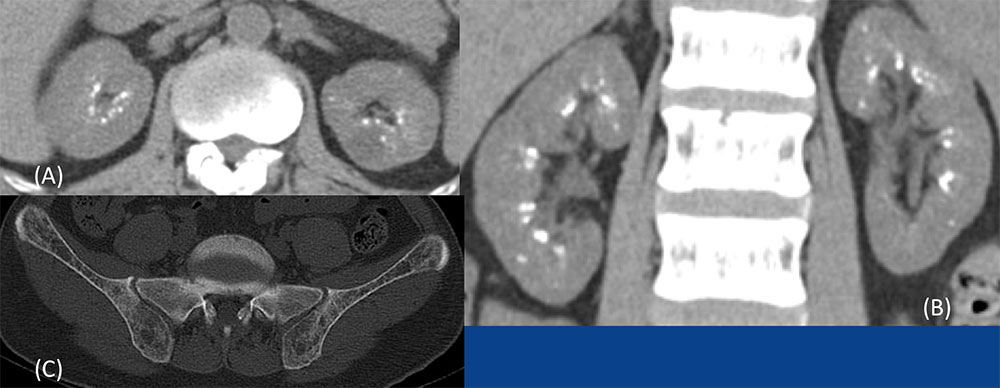 40-year-old male with prior resection of parathyroid carcinoma, presented with lung metastases and recurrent hyperparathyroidism. (A) Axial and (B) coronal noncontrast CT show multiple calcifications in the medulla. (C) Diffuse demineralization of pelvic bones. |
Medullary Nephrocalcinosis 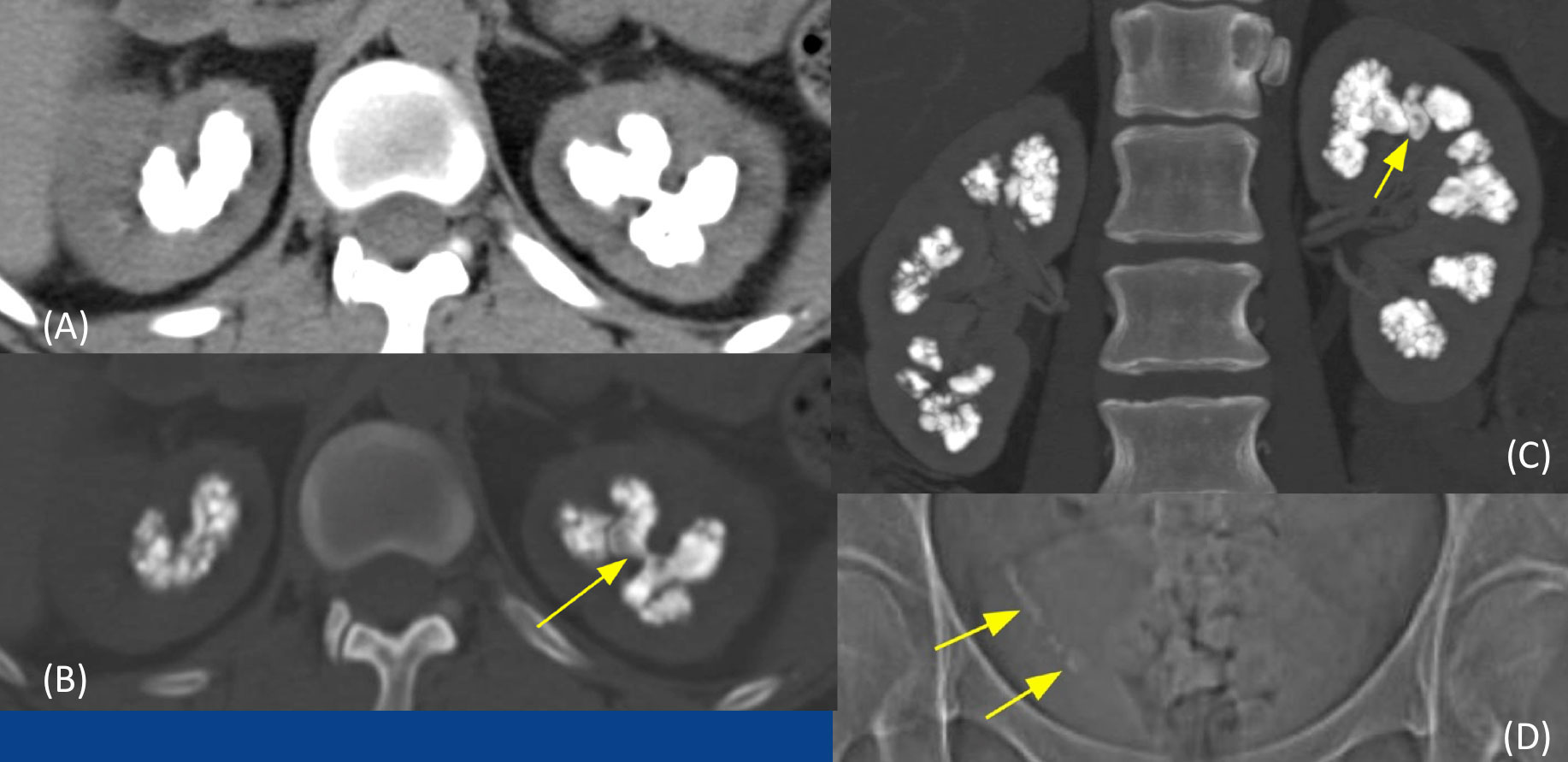 40-year-old woman with renal tubular acidosis type 1 (distal). History of renal stones, recurrent UTIs, presented with right flank pain. (A) Noncontrast axial soft tissue window and (B) wide window images, and (C) coronal postcontrast MIP image show massive calcifications in the renal medulla. A calculus fills the upper pole calyx (yellow arrow) is also seen (B, C). (D) Scout image shows multiple calculi in the distal right ureter (yellow arrows). Renal tubular acidosis Type 1 (distal): When massive medullary nephrocalcinosis is seen, renal tubular acidosis is usually the underlying cause. |
Papillary Necrosis
|
Papillary Necrosis 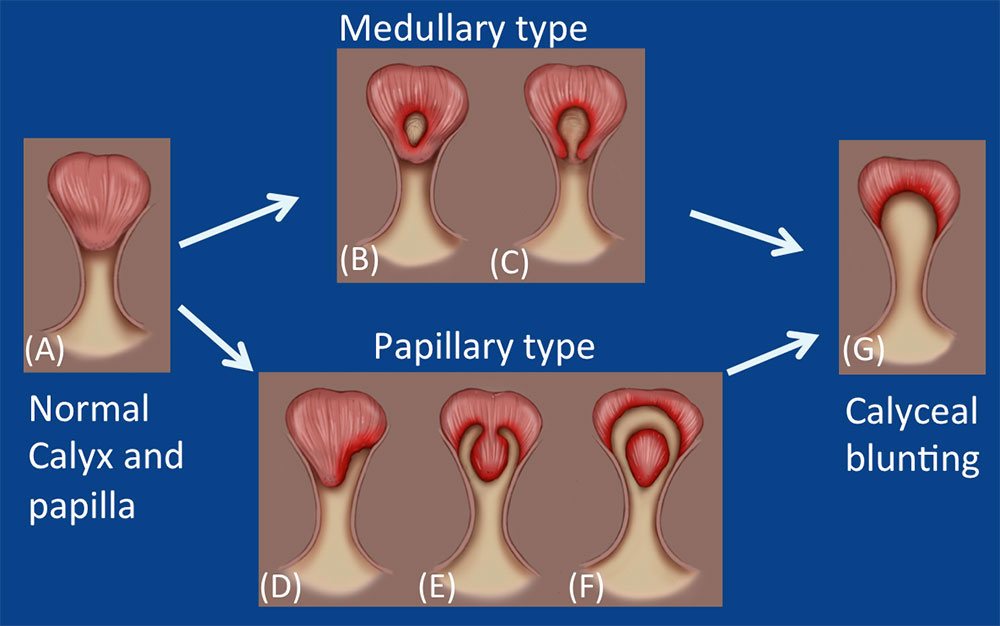 (A) Normal calyx and papilla (B, C) Medullary types: central erosion of the papilla Central erosion of the papilla with ball on tree appearance (D, E, F) Papillary types: entire papilla may become necrotic (D) Unilateral forniceal erosion (E) Bilateral forniceal erosions with lobster claw appearance (F) Necrotic papilla retained in calyx after sloughing (G) Calyceal blunting and epithelialization Typical progression of papillary necrosis: 1. Reversible ischemic change 2. Necrosis and sloughing of papillary tissue into the pelvocalyceal systems 3. Contrast material-filled papillary cavities 4. Blunting of calyces |
Papillary Necrosis 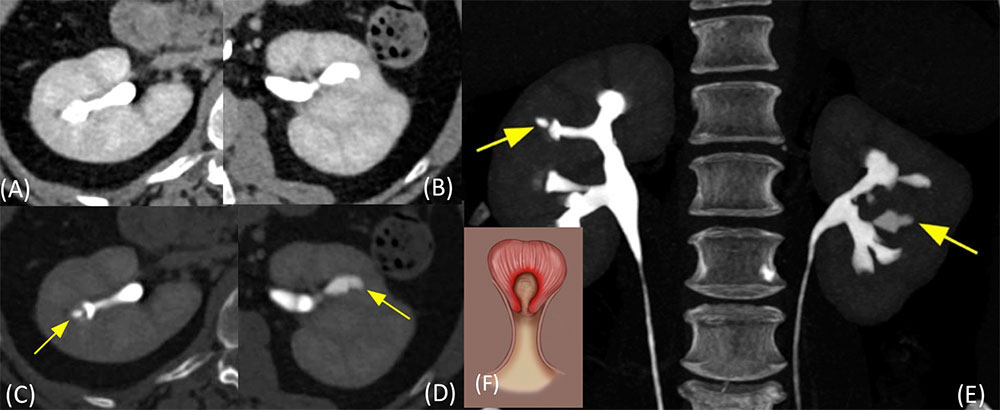 60-year-old woman with microscopic hematuria. History of migraine headaches and using analgesics. Papillary necrosis: Central erosion of papilla is known as the medullary type of papillary necrosis. It may have “ball on tree” appearance (Figure F). |
Renal Abscess and Papillary Necrosis 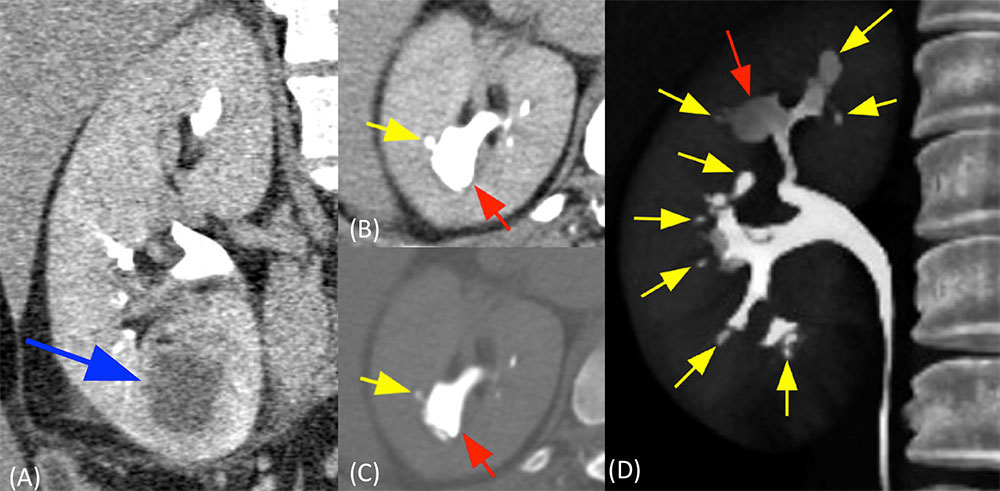 46-year-old woman with history of multiple prior UTIs, presented with renal abscess. |
Papillary Necrosis with Sloughed Papilla 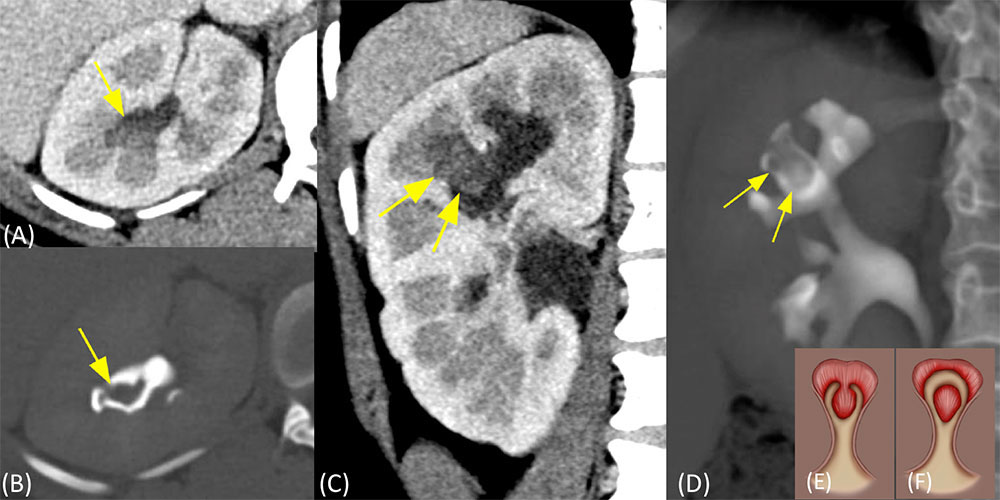 Papillary necrosis: In the papillary type, the entire papilla may become necrotic and slough. It may have “lobster claw” appearance |
Papillary Necrosis with Sloughed Papilla 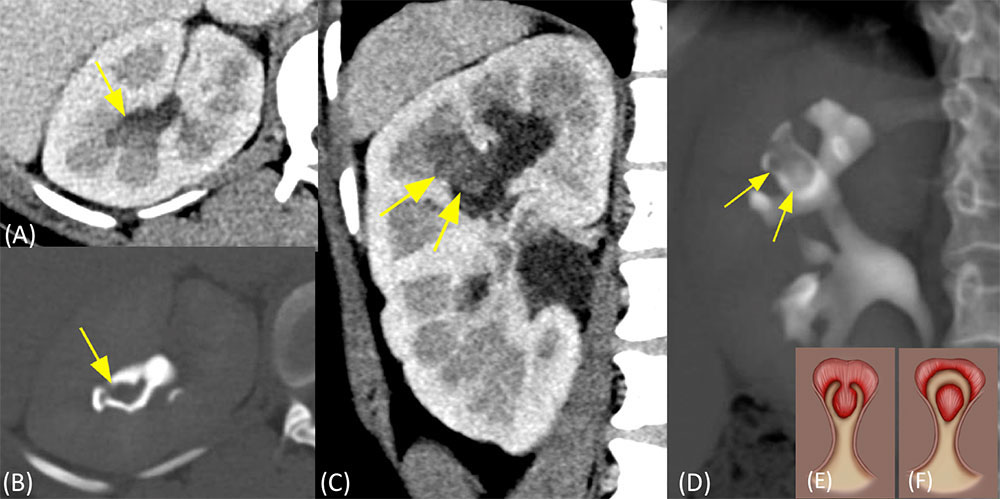 28-year-old woman with history of sickle cell disease, presented with hematuria and abdominal pain. (A) Axial and (C) coronal images in corticomedullay phase show soft tissue density filling defect in the blunted upper pole calyx (yellow arrows). It is seen as a filling defect in excretory phase (B) axial and (D) coronal volume rendered images, representing sloughed papilla. Papillary necrosis: In the papillary type, the entire papilla may become necrotic and slough. It may have “lobster claw” appearance (Figure E). |
Renal and Urinary Tract Tuberculosis 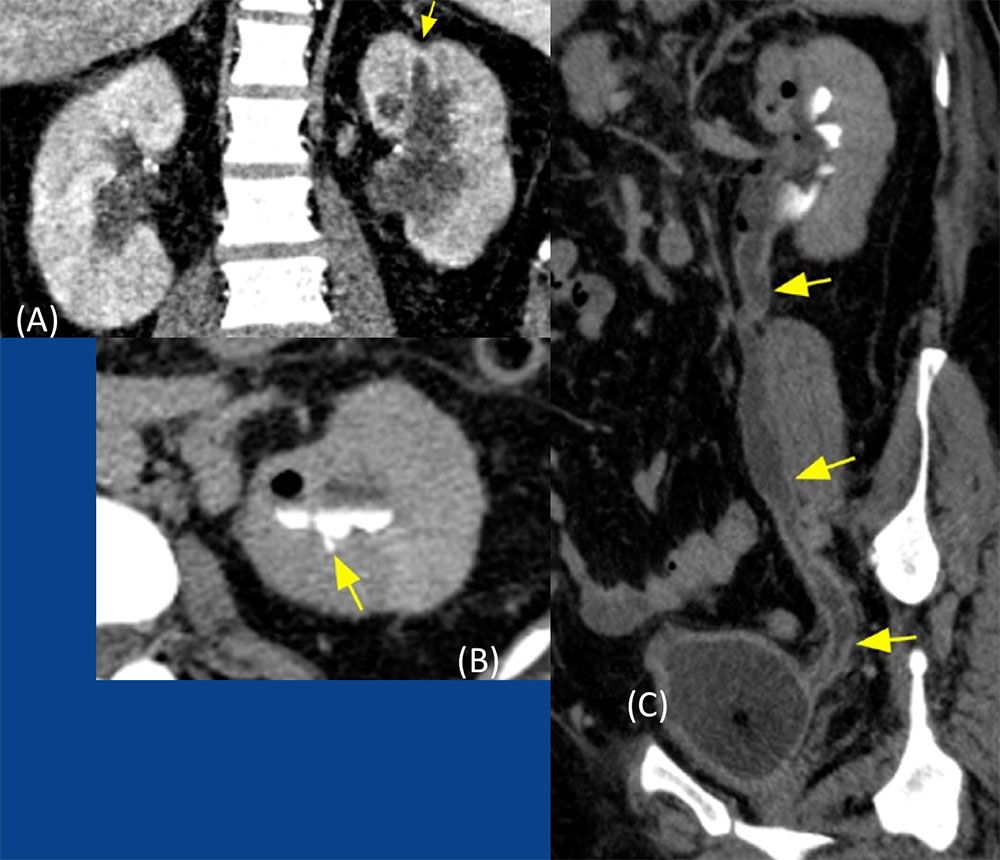 Renal and urinary tract tuberculosis . (A) Coronal nephrographic phase image shows thickening and blunting of the upper pole calyx with adjacent cortical scarring (arrow). (B) Axial excretory phase image shows small contrast collection in the area of papilla (arrow), indicating small papillary necrosis. (C) Excretory phase oblique sagittal image shows diffuse irregular wall thickening and enhancement of the left ureter and bladder with long-segment ureteral narrowing. Genitourinary tuberculosis: Accounting for 15–20% of tuberculous infections outside lungs It results from hematogenous seeding of bacilli in the glomerular and peritubular capillary bed. Regional spread of bacilli results into seeding into the renal pelvis, ureters and bladder. |
Calyceal Diverticulum 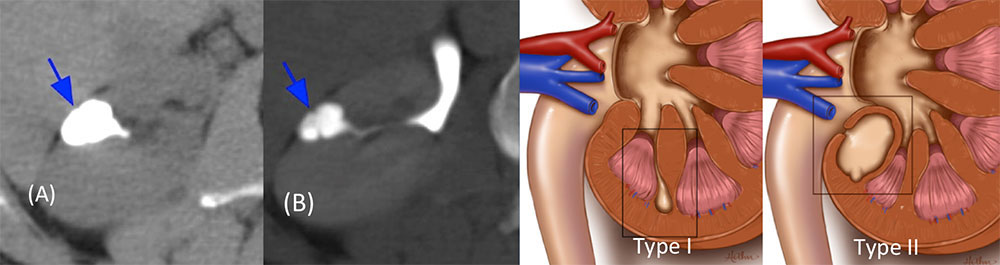
|
Calyceal Diverticulum 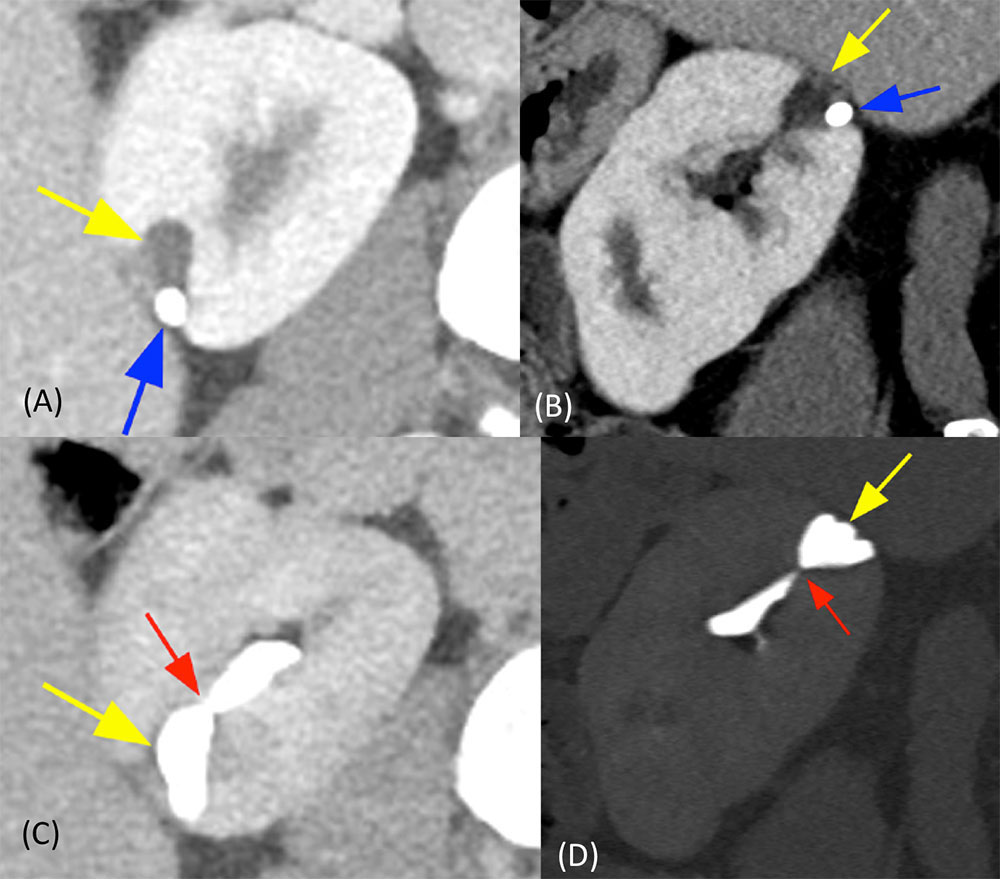 53-year-old male with incidental small calyceal diverticulum. (A) Axial and (B) sagittal nephrographic phase CT images show a small cystic lesion in the right kidney (yellow arrow) containing a small calculus (blue arrow). (D) Axial and (E) sagittal excretory phase CT images show contrast accumulation within a diverticulum (yellow arrow) which communicates with a calyx with a narrow isthmus (red arrow). |
Summary
|
