Renal Papillary and Calyceal Lesions on CT UrographyRenal Papillary and Calyceal Lesions on CT Urography Satomi Kawamoto, M.D The Russell H. Morgan Department of Radiology and Radiological Science and Department of Pathology Johns Hopkins Medical Institutions Baltimore, MD USA |
Purpose/Educational Goals
|
Outline
|
Renal Vascular and Renal Tubular Anatomy 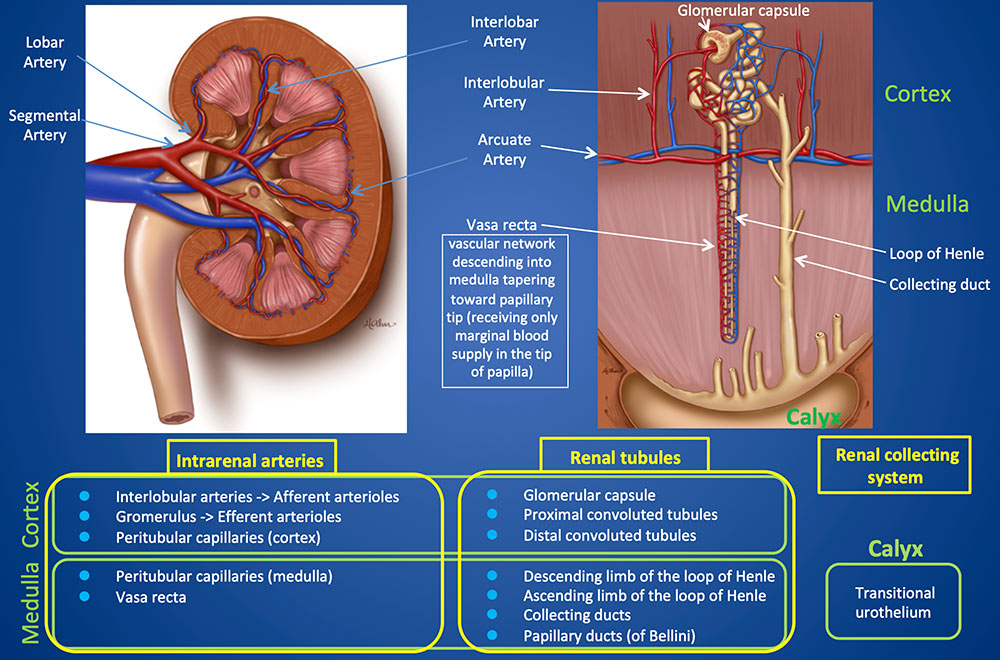 |
Normal Renal Enhancement on CT 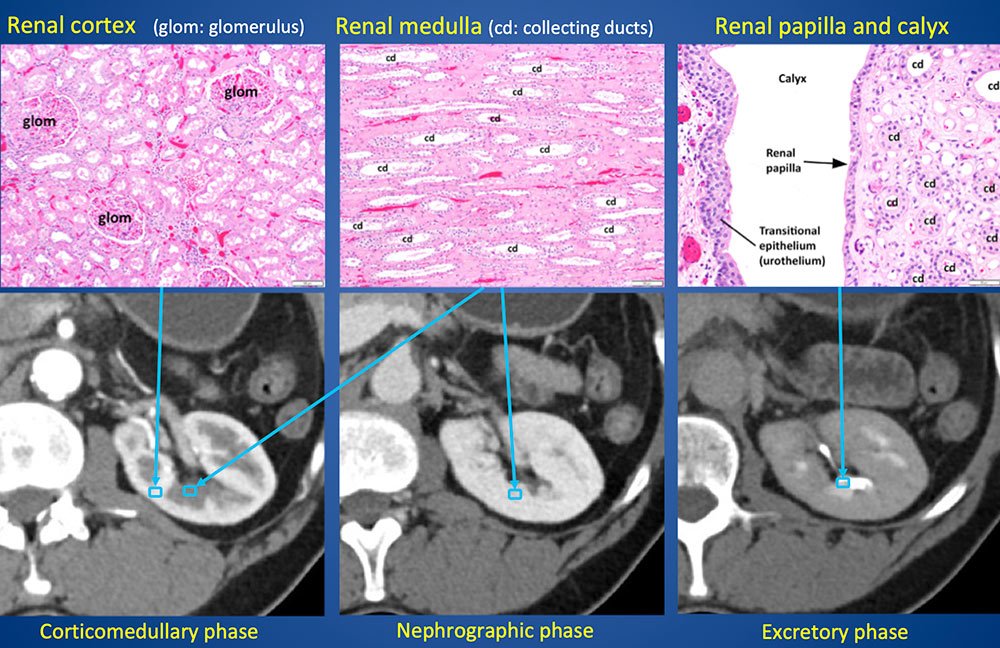 |
Normal Anatomy of Renal Collecting System 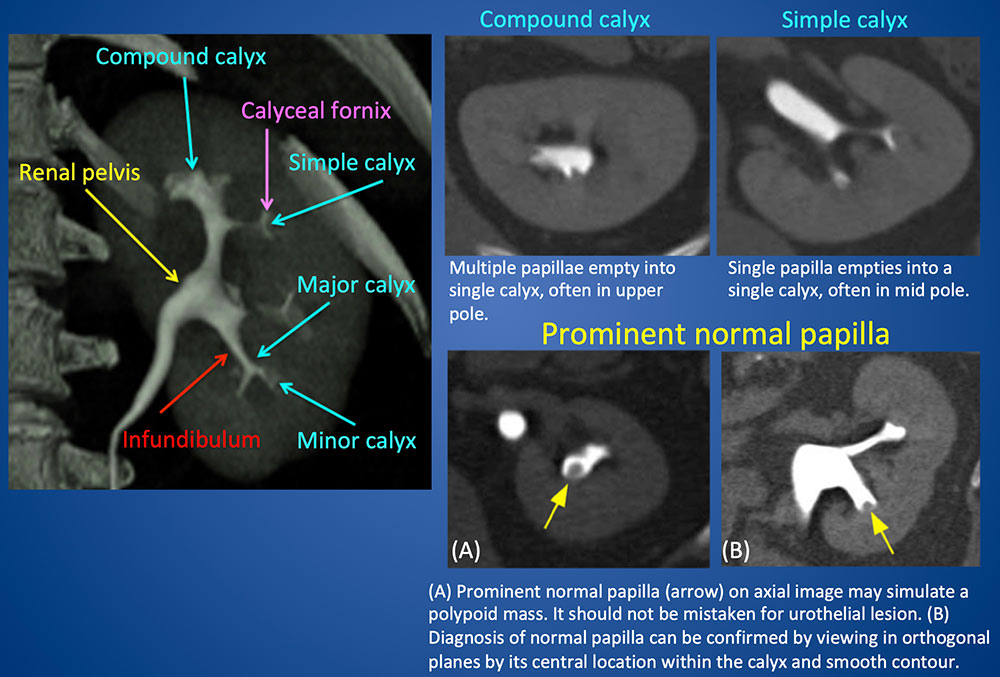 |
Normal Papillary Blush Normal papillary blush in an asymptomatic patient. (A) Early excretory phase axial CT in soft tissue window, and (B) axial and (C) coronal wide window images show indistinct, prominent papillary opacity in “blushlike” appearance (arrows), representing normal concentration of contrast in the medulla. Normal papillary blush is accentuated with low-osmolality contrast media (less fluid is excreted into the tubular lumen, therefore the concentration of contrast material is higher than with high-osmolality contrast material). 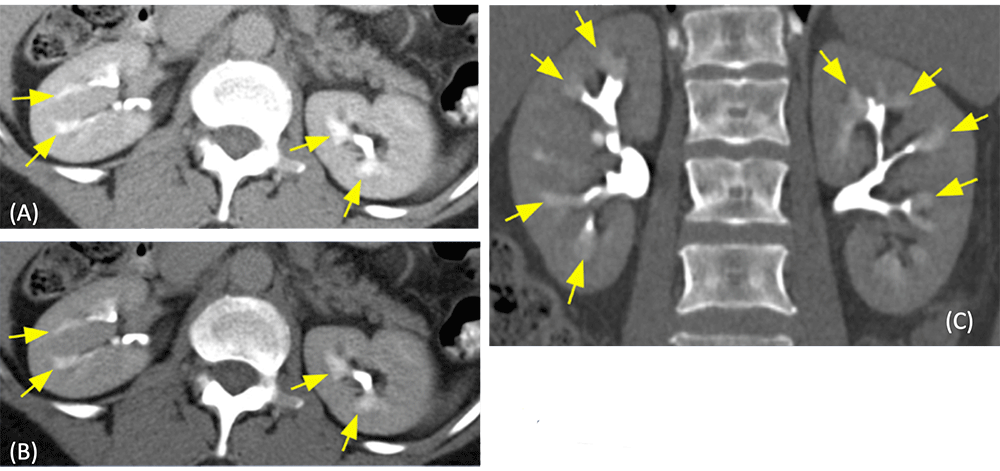 |
Benign Tubular Ectasia 55-year-old man with benign tubular ectasia, presented with microscopic hematuria. Excretory phase CT images show distinct, linear, “paintbrush”-like collections of contrast (arrows) in the dilated collecting ducts in the renal pyramids, which are difficult to appreciate on soft tissue window (A), and better appreciated in wide window image (B) and coronal MIP image (C). 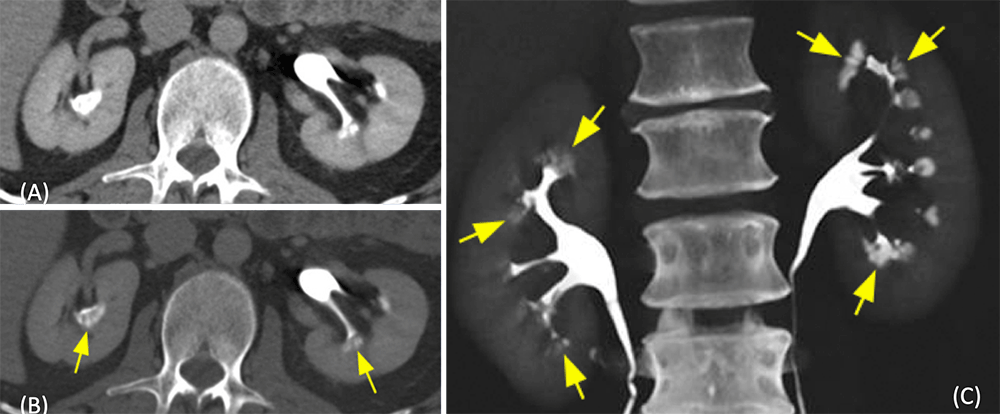 |
Medullary Sponge Kidney 40-year-old man with history of renal stones and hematuria. (A) Noncontrast CT shows a small calcification in the papilla (red arrow). (B) Excretory phase CT in soft tissue window shows no obvious abnormality. However, in wide window image (C) and coronal MIP image (D) show “paintbrush” appearance of the medullary pyramids (yellow arrows) due to pooling of contrast within the dilated collecting ducts, a finding typical of medullary sponge kidney. 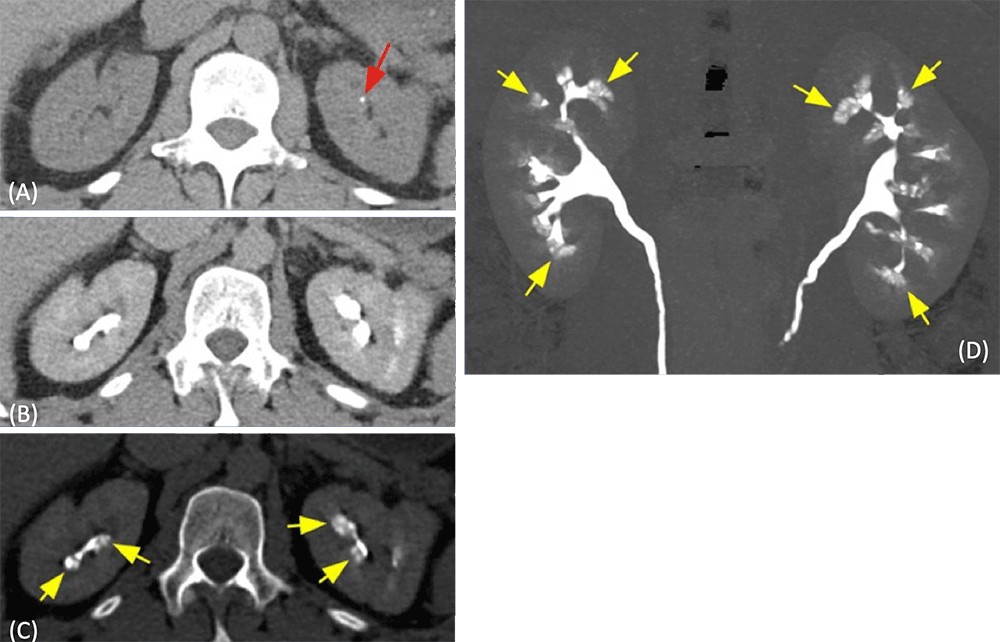 |
Benign Tubular Ectasia/Medullary Sponge Kidney
|
Medullary Nephrocalcinosis 40-year-old male with prior resection of parathyroid carcinoma, presented with lung metastases and recurrent hyperparathyroidism. (A) Axial and (B) coronal noncontrast CT show multiple calcifications in the medulla. (C) Diffuse demineralization of pelvic bones. (D, E) Multiple lung metastases (arrows). Parathyroid carcinoma is less than 1% of all causes of hyperparathyroidism. 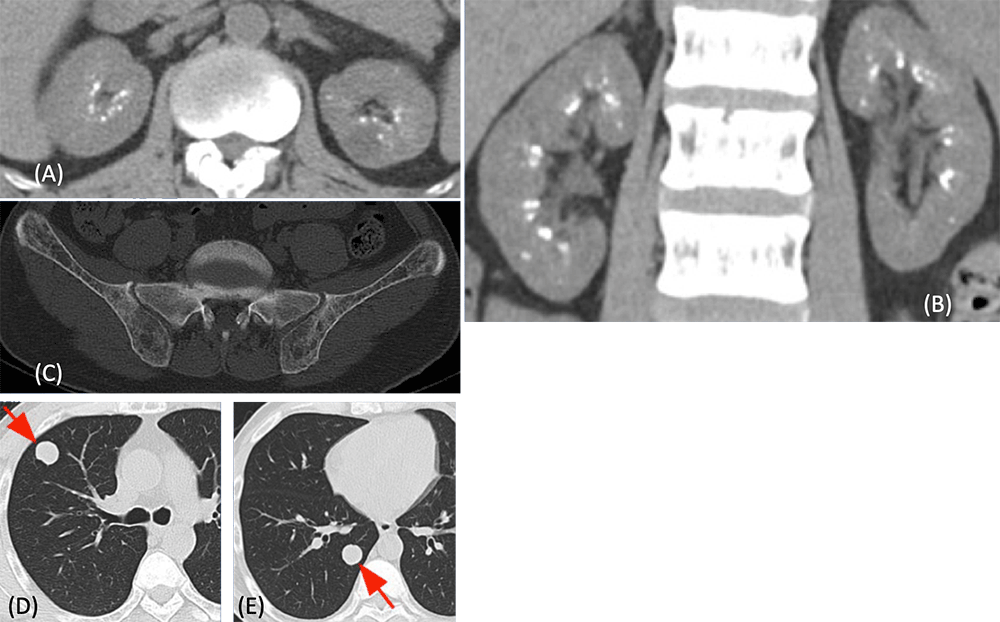 |
Medullary Nephrocalcinosis 40-year-old woman with renal tubular acidosis type 1 (distal). History of renal stones, recurrent urinary tract infections (UTIs), presented with right flank pain. (A) Noncontrast axial soft tissue window and (B) wide window images, and (C) coronal postcontrast MIP image show massive calcifications in the renal medulla. Calculus filling the upper pole calyx (yellow arrow) is also seen. (D) Scout image shows multiple calculi in the distal right ureter (yellow arrows). Renal tubular acidosis Type 1 (distal)
 |
Medullary Nephrocalcinosis
|
Papillary Necrosis 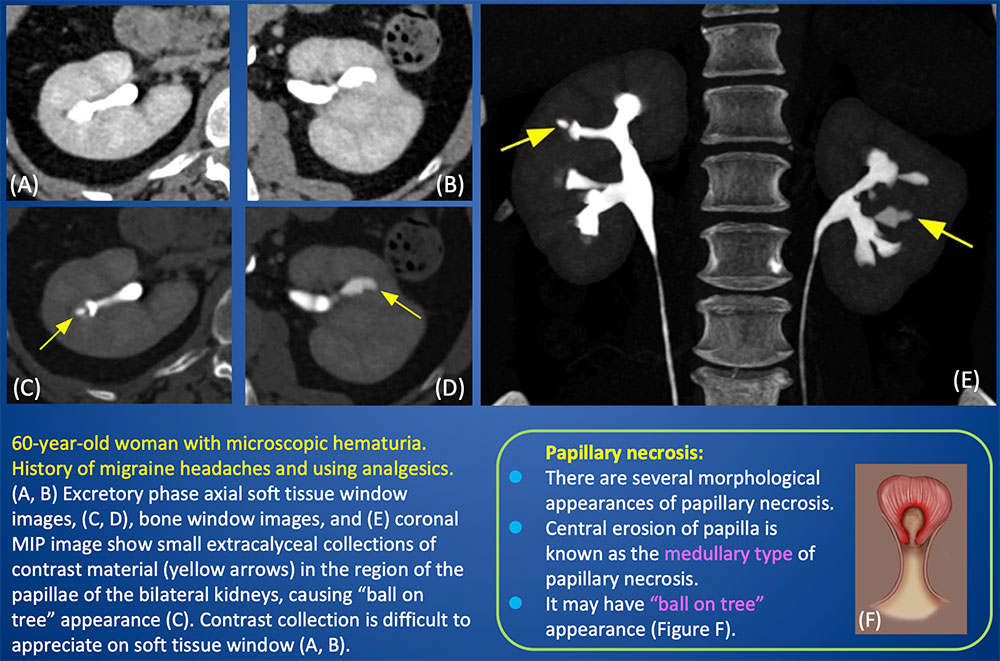 |
Renal Abscess and Papillary Necrosis 46-year-old woman with history of multiple prior UTIs, presented with renal abscess. (A) Coronal excretory phase CT shows renal abscess (blue arrow). (B) Axial excretory phase soft tissue window and (C) wide window images, as well as (D) coronal MIP image show dilated blunted upper pole calix (red arrow) with multiple collections of contrast in “ball on tree” appearance (yellow arrows) representing papillary necrosis. Wide window and MIP images better demonstrate contrast collections than soft tissue window. 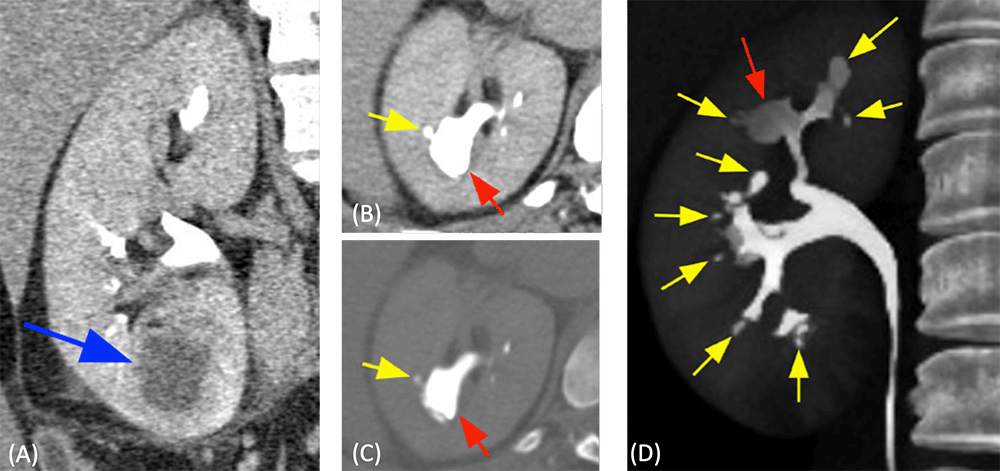 |
Papillary Necrosis with Sloughed Papilla 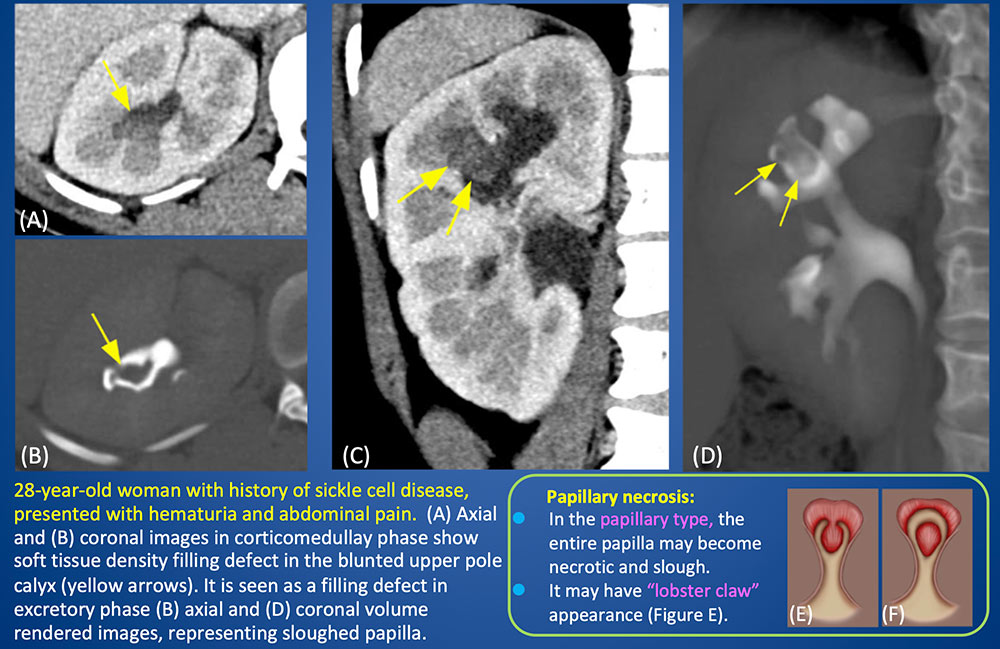 |
Renal and Urinary Tract Tuberculosis Renal and urinary tract tuberculosis (Tbc). (A) Coronal nephrographic phase image shows thickening and blunting of the upper pole calyx with adjacent cortical scarring (arrow). (B) Axial excretory phase image shows small contrast collection in the area of papilla (arrow), indicating small papillary necrosis. (C) Excretory phase coronal and (D) oblique sagittal images show diffuse irregular wall thickening and enhancement of the left ureter and bladder with long-segment ureteral narrowing. (Images curtesy of Dr. Zubair Kazi, Consultant Radiologist, Saifee Hospital) Genitourinary tuberculosis (Tbc):
 |
Papillary Necrosis
|
Papillary Necrosis 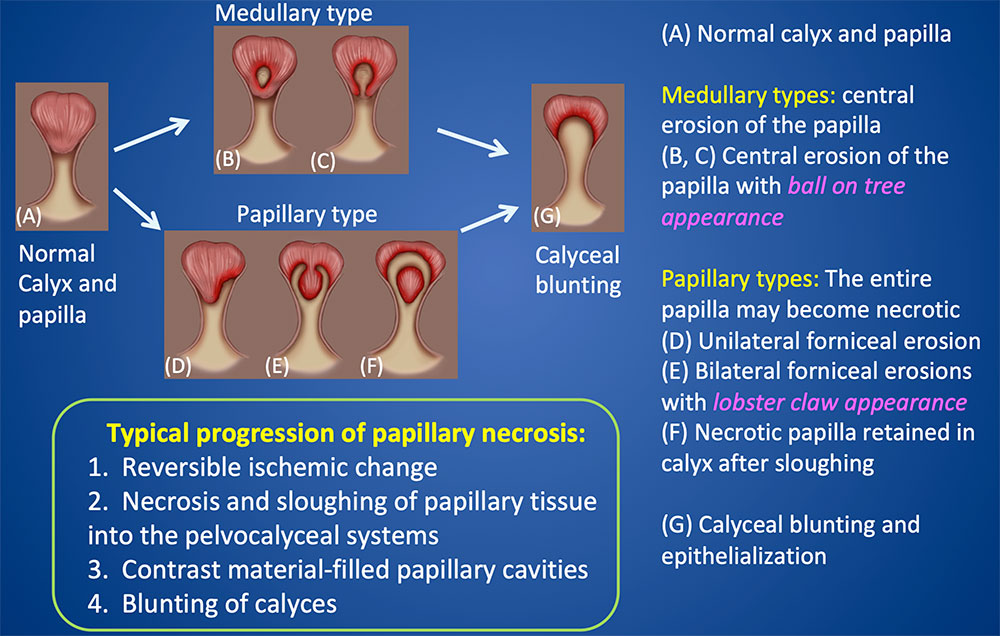 |
Calyceal Diverticulum 20-year-old woman with recent history of UTI. (A, B) Axial CT images in late corticomedullary phase shows complex cystic lesion (yellow arrows) in the right kidney, containing a calcification (blue arrow). Excretory phase axial images (C, D) and MIP image (E) show contrast accumulation within the cystic lesion (yellow arrows) surrounding the calcification (blue arrow), representing a calyceal diverticulum with a calculus. 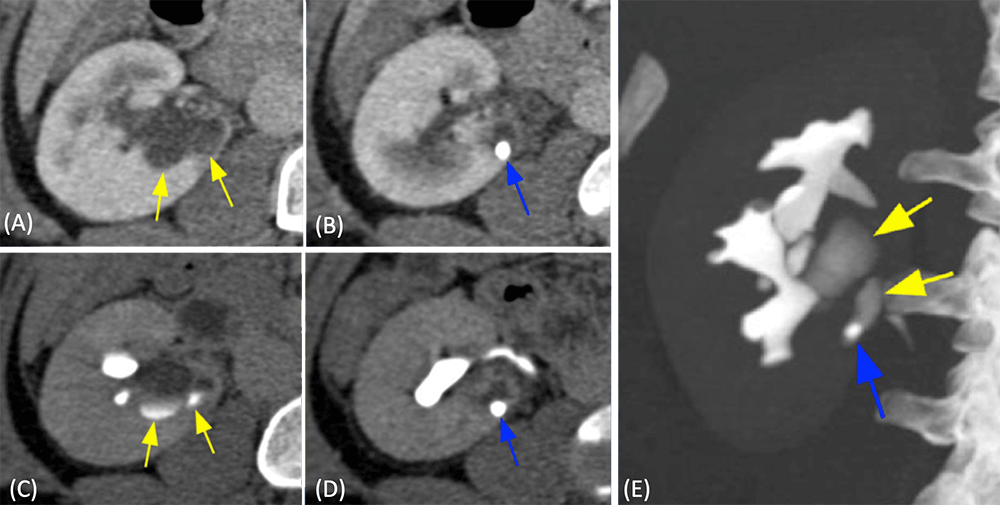 |
Calyceal Diverticulum 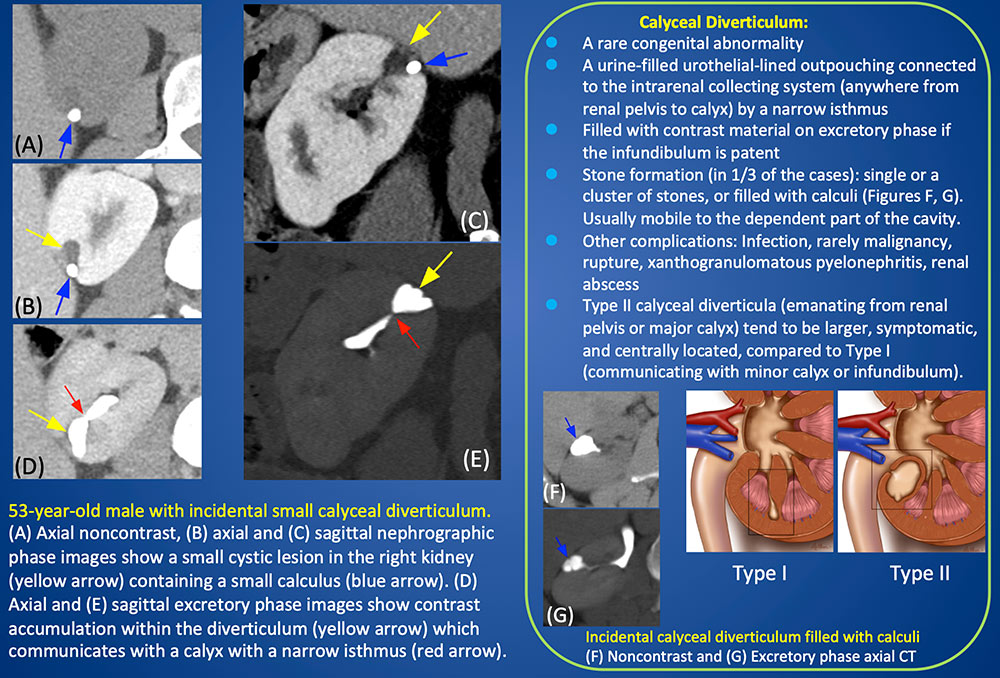 |
Hydronephrosis and Forniceal Rupture 85-year-old male with colon cancer with pelvic metastasis resulting in right hydronephrosis. (A) Axial late nephrographic phase CT shows right hydronephrosis with decreased contrast enhancement of the right kidney compared to the left. (B) Axial, (C) coronal, and (D) sagittal excretory phase CT images show contrast leakage from calyceal fornix, with extravasated contrast surrounding the right renal pelvis and proximal ureter (yellow arrows). Contrast excretion within the renal calyces is also seen (red arrows).  |
Forniceal Rupture
|
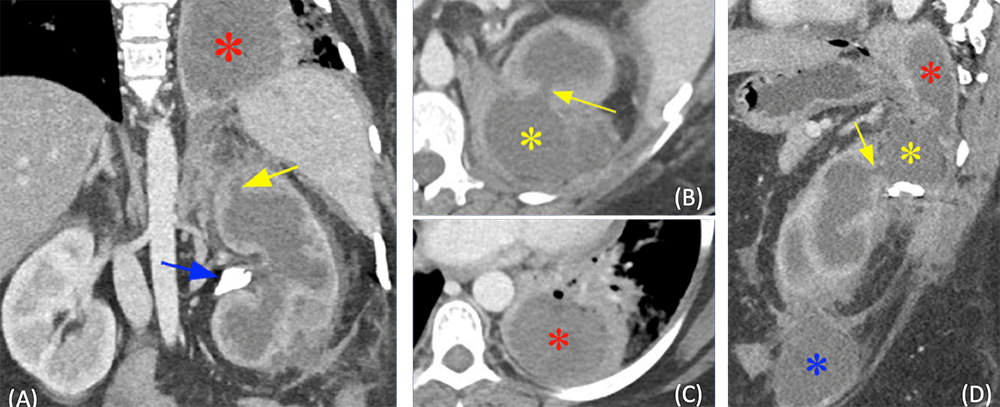
Xanthogranulomatous Pyelonephritis (XGP) with Ruptured Calyx and Perinephric and Intrathoracic Extension 42-year-old woman with XGP, presented with chronic left flank pain. (A) Coronal contrast enhanced CT shows poorly functioning left kidney with a large obstructing calculus (blue arrows) and large central hypodense areas due to dilated collecting system, representing XGP. (B, C) Axial and (D) oblique sagittal contrast enhanced CT show perirenal abscess (yellow asterisk) through the calyceal defect (yellow arrow) with intrathoracic extension (red asterisk). Additional perirenal abscess is also seen more inferiorly (blue asterisk). Xanthogranulomatous Pyelonephritis :
 |
Pyonephrosis and Fistulous Connection between Renal Calyx and Perinephric/Abdominal Wall Abscess 56-year-old woman with history of renal calculi and recurrent UTIs, who presented with urosepsis. (A) Oblique coronal, (B) axial, and (C) oblique sagittal contrast enhanced CT images show obstructing distal ureteral calculi (green arrow) with hydronephrosis. Fistulous connection (yellow arrow) from the dilated calyx to perinephric and abdominal wall abscess (red arrows) containing a calculus (B: blue arrow). Multiple renal calculi are also seen in the dilated calyces (blue arrows). (D) Longitudinal gray-scale ultrasonography shows layering debris (yellow arrows) within the dilated renal collecting system, suggesting presence of pus. 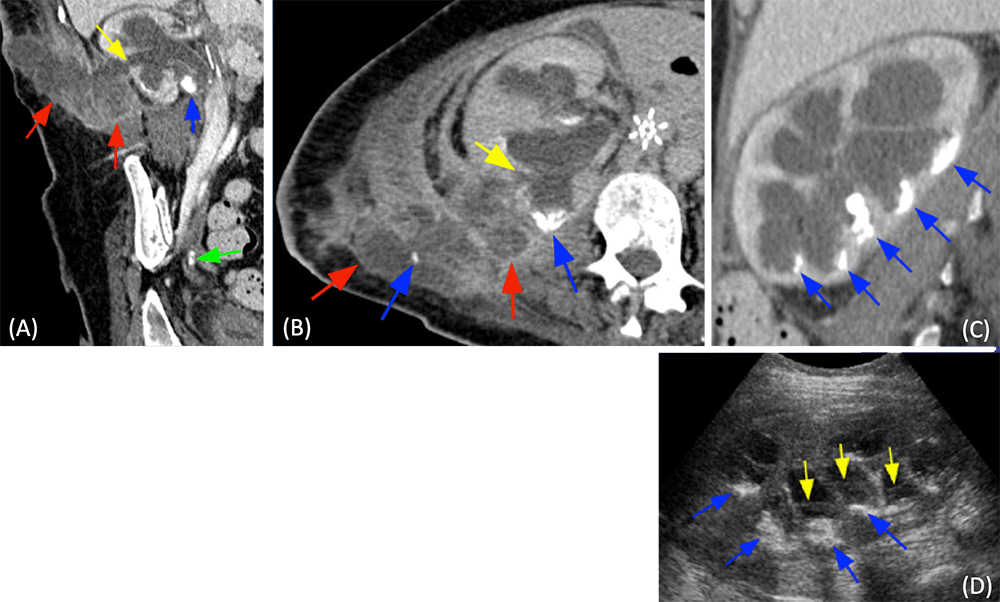 |
Pyonephrosis
|
Acute Pyelonephritis, Pyelitis, Ureteritis, Cystitis 40-year-old woman with HIV and UTI. Urine culture grew E.coli. (A) Coronal corticomedullary phase CT image shows diffuse wall thickening of calyces and renal pelves (yellow arrows) representing pyelitis. Wedge shaped hypodense lesions in the right kidney (red arrows) representing acute pyelonephritis. (B, C) Axial arterial phase and (D) excretory phase images show diffuse thickening of the ureters (yellow arrows) and bladder (red arrow) with mucosal enhancement due to ureteritis and cystitis. 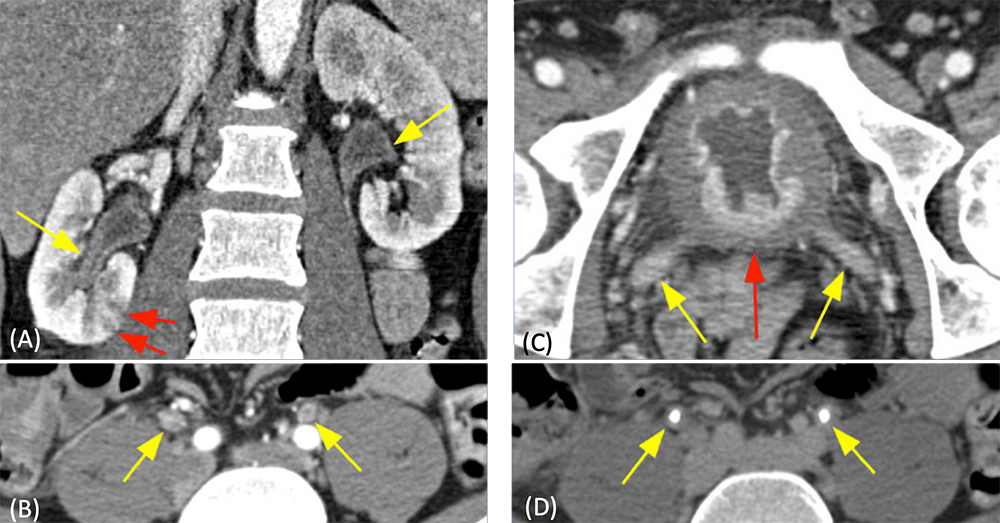 |
Acute Pyelonephritis, Emphysematous Pyelitis 58-year-old woman with history of diabetes mellitus, nausea, vomiting, and right upper quadrant pain. (A, B) Axial contrast enhanced CT in delayed phase (several hours after IV contrast administration) show enlarged right kidney with hydronephrosis, and delayed excretion of contrast from the right kidney due to obstructing distal right ureteral calculus (not shown). Air within the lumen and wall of the right renal collecting system (yellow arrows). Multifocal areas of decreased enhancement (red arrows) related to acute pyelonephritis. E. Coli grew in the blood and urine cultures. The patient underwent right nephrectomy. Perinephric abscess and severe multifocal acute pyelonephritis were found pathologically. 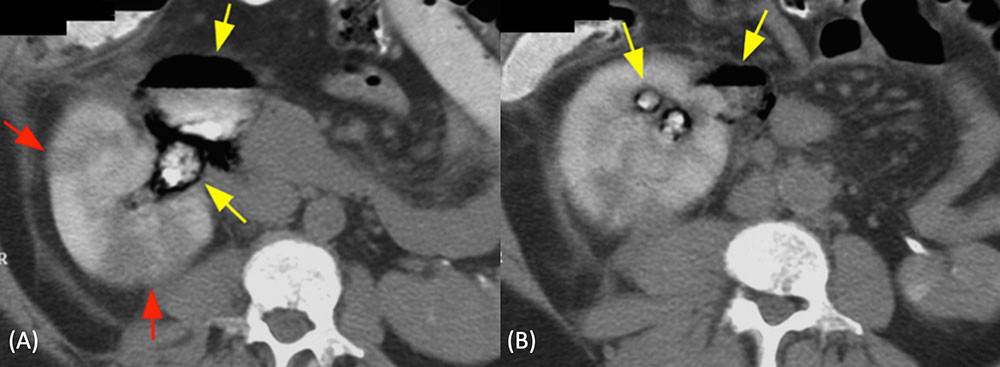 |
Emphysematous Pyelonephritis
|
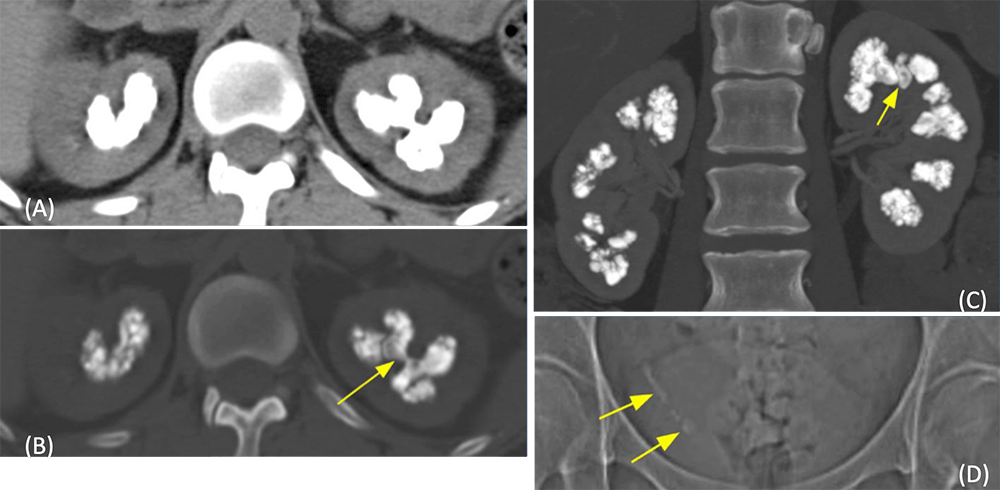
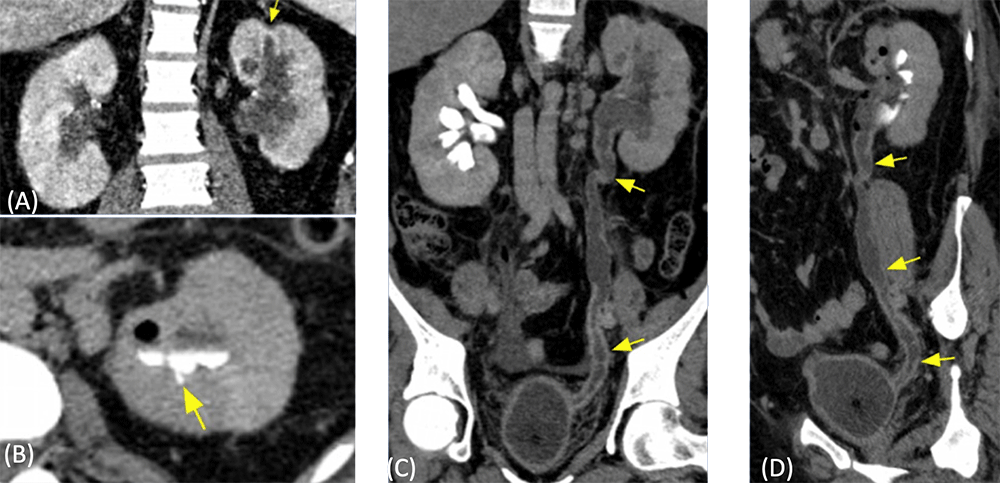
Renal Atrophy and Calyceal Clubbing 21-year-old woman with spina bifida, neurogenic bladder, status post bladder augmentation at age 7 with multiple revisions and ureteral re-implant. Recurrent stones and UTIs. (A) Axial corticomedullary phase, and (B) axial and (C) coronal excretory phase images show atrophic right kidney with severe parenchymal scarring with loss of medulla and cortex over the calyceal clubbing (arrows). Irregular bladder contour (asterisk) due to multiple prior surgeries. 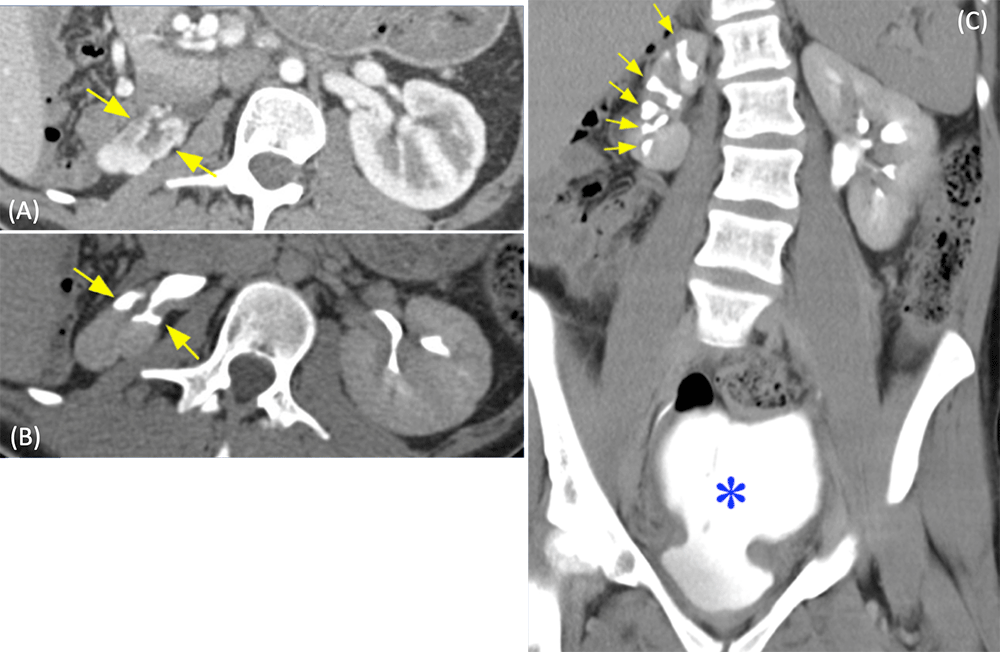 |
Urothelial Carcinoma 89-year-old woman presented to emergency room for gross painless hematuria. (A) Axial and (B) coronal corticomedullary phase images show a subtle enhancing mass in the lower pole calyceal region. The mass encases and narrows the lower pole calyx on excretory phase (C) axial and (D) coronal CT. Pathology revealed high grade urothelial carcinoma which invaded deeply into the renal cortex to within 2 mm of the renal capsule (pT3). 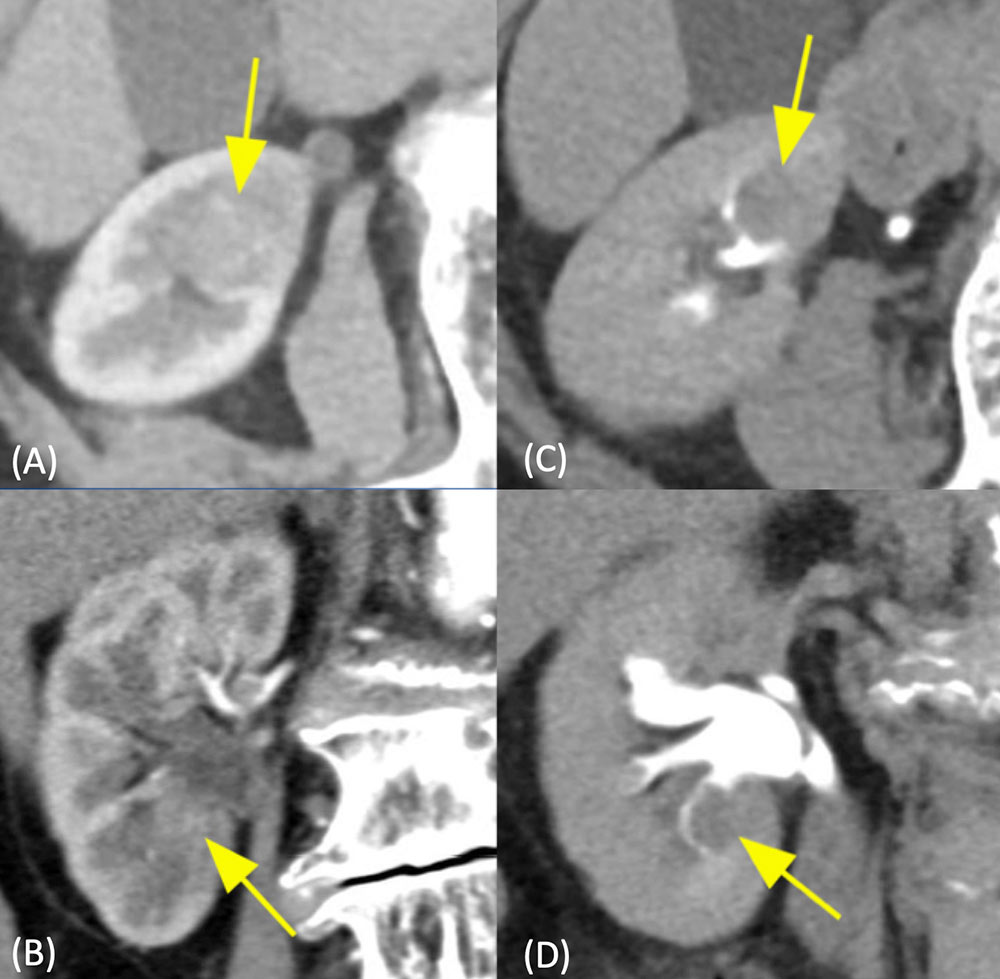 |
Multifocal Urothelial Carcinomas 63-year-old man with history of bladder cancer. Multifocal urothelial carcinomas of the right renal collecting system. (A, B) Axial corticomedullay phase images shows a mass in the upper pole calyx (yellow arrow in Figure A) and mid pole calyx (red arrow in Figure B). On excretory phase axial images (C, D) and anterior volume rendered image (E), these masses are seen as filling defects (yellow and red arrows). Additional multiple filling defects are also present in the renal collecting system (arrowheads in Figure E). The patient underwent right ureteronephrectomy, which revealed multifocal papillary urothelial carcinomas. 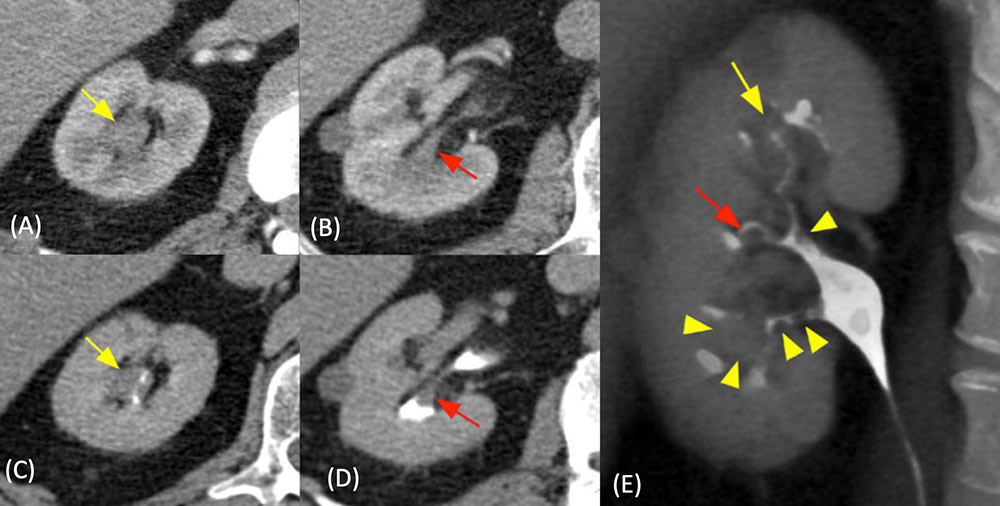 |
Urothelial Neoplasm
|
Summary
|
References
Acknowledgements
|
